Blood:MiR-125a和miR-34a可预测CLL患者是否发生Richter综合征
2018-09-22 MedSci MedSci原创
中心点:MiR-125a-5p高表达或miR-34a-5p低表达可预测约50%的RS,假阳性率9%。MiR-125a-5p和miR-34a-5p可作为预测CLL患者有无RS发展的标志物。摘要:慢性淋巴细胞白血病(CLL)是一种最常见的成人白血病。其特点是CD19+/CD5+淋巴细胞积累,预后多变。Richter综合征(RS)是CLL患者的一种致命性并发症,可导致侵袭性B细胞淋巴瘤。迄今为止,尚无检
MiR-125a-5p高表达或miR-34a-5p低表达可预测约50%的RS,假阳性率9%。
MiR-125a-5p和miR-34a-5p可作为预测CLL患者有无RS发展的标志物。
摘要:
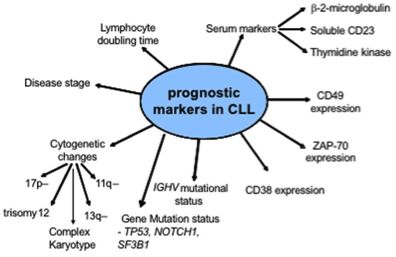
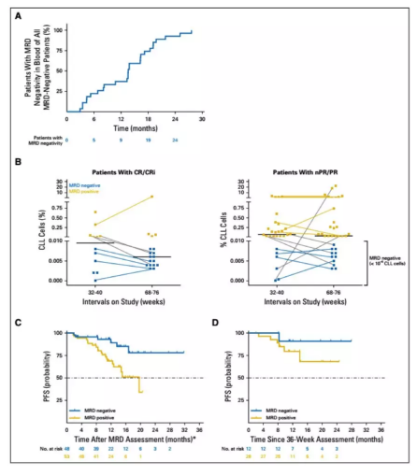
慢性淋巴细胞白血病(CLL)是一种最常见的成人白血病。其特点是CD19+/CD5+淋巴细胞积累,预后多变。Richter综合征(RS)是CLL患者的一种致命性并发症,可导致侵袭性B细胞淋巴瘤。迄今为止,尚无检验可预测RS的发生。鉴于microRNA表达的癌变可预测多种癌症的进展侵袭,Veronica Balatti等人探究是否存在特异性的microRNA调控异常,可预测CLL患者发生RS。
研究人员将49位出现RS的CLL患者的样本的microRNA的表达水平与59位无RS的CLL患者的样本的microRNA的表达水平进行对比,发现miR-125a-5p高表达或miR-34a-5p低表达可预测约50%的RS,假阳性率9%。与对照组相比,RS患者miR-125a-5p的表达水平升高了20倍、miR-34a-5p的表达水平降低了21倍。
因此,研究人员推测miR-125a-5p和miR-34a-5p可作为预测RS的标志物,有潜力为临床医生提供有用的信息,有助于为CLL患者制定最佳的治疗方案。
Veronica Balatti, et al. MiR-125a and MiR-34a expression predicts Richter syndrome in chronic lymphocytic leukemia patients. Blood 2018 :blood-2018-04-845115; doi: https://doi.org/10.1182/blood-2018-04-845115
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Richter综合征#
38
#miR#
32
#miR-34a#
37
#ICH#
28
#综合征#
24
了解一下谢谢
61