Nat Commun:德国科学人员“揪出”癌症转移的罪魁祸首,新疗法有希望了
2018-03-02 佚名 medicalxpress
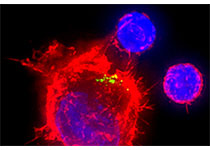
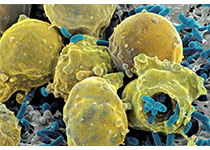
德国癌症研究中心的科学家在《自然通讯》的报告中指出,癌细胞转移的风险不仅仅在于他们的数量,而且还在于他们的特点,癌细胞为了循环侵入组织并在体内其他部位定居,它们必须表现出特定的极性。这一发现可能有助于更好地预测转移的个体风险,并找到适当的治疗方法,以减少转移。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#COMMUN#
37
#Nat#
33
想法很好.
56
#癌症转移#
39
#德国#
33
#新疗法#
21
学习了.涨知识
56