CLIN CHEM LAB MED:系统性硬化症患者的原发性胆道胆管相关血清学特征
2020-03-21 MedSci原创 MedSci原创
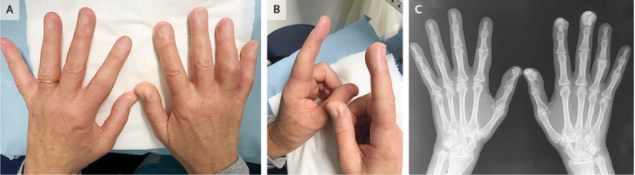
自身免疫性疾病--系统性硬化(SSc)和原发性胆道胆管炎(PBC)可能同时发生,且与疾病特异性自身抗体密切相关。
自身免疫性疾病--系统性硬化(SSc)和原发性胆道胆管炎(PBC)可能同时发生,且与疾病特异性自身抗体密切相关。本研究探讨了PBC特异性血清学(PBC-Ab)的患病率和特异性,以及与SSC亚型和SSC特异性抗体的关系,以及与胆汁淤积性肝酶的关系。比较了三种不同的检测方法。
研究人员用间接免疫荧光法(II F)分析人上皮瘤-2000(Hep-2000)细胞(ANA-IIF,免疫概念)和肝肾上腺样组织切片(II F-LKS)(Menarini),以及免疫印迹(L B)。在第一次取样(T0)和随访3年(T3)时对碱性磷酸酶/γ-谷氨酰转移酶(ALP/GGT)进行评价。
研究发现,在13%的患者中存在PBC-Ab,与着丝粒抗体(anti-CENP-B)显著相关,但与限制性皮肤SSC亚群(Lcssc)无关。反应最频繁的是AMA(11%,其中AMA- m2占9%)和Sp-100抗体(5%),显示出主要的重叠。在t0和t3时,PBC-Ab的存在与ALP或GGT升高之间没有相关性。使用IIF-LKS检测AMA可与LB相比较。与LB相比,ANA-IIF筛选的敏感性较低。
研究表明,即使经过3年的随访,在没有胆汁淤积肝酶升高的情况下,在SSc中仍可检测到广泛的PBC-Ab。然而,由于这些抗体可能先于PBC疾病达10年,我们的队列需要进一步的前瞻性随访。
原始出处:
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#硬化症#
40
#原发性#
39
#系统性#
44
#血清学#
46
#Med#
39
#系统性硬化#
40
#胆管#
29