Sci Rep:人类耳蜗组织病理学反应了主要神经退化的临床特征
2017-07-20 AlexYang MedSci原创
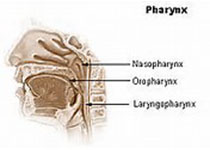
听觉神经病变是一种显著的和正在研究的人类听力损失的起因,不管感觉细胞典型功能,可在表现为异常耳蜗神经功能的病人中诊断。因为人类内耳在活人中不可能可视化,尸检标本的组织病理学分析对理解该病理的细胞机制非常重要。最近,有研究人员展现了重度主要神经退化的统计学模型,并且阐释了该病病理与纯音听力测定阈值和言语识别得分的关系,并与年龄相匹配的对照组进行比较,且每10年进行数据生成。研究发现,从23名病人的3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#临床特征#
36
#组织病理学#
36
henhao
55
学习了谢谢分享
64
学习了很有用
57
好东西学习了!
47
#病理学#
31