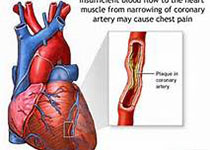
JACC:右心疾病通过影响纤维化和传导系统促进房颤的形成
2019-09-13 不详 MedSci原创
影响右心的疾病会促进房颤的形成,但具体机制尚不清楚。本研究的目的旨在通过肺动脉高压(PH)大鼠模型探究右室疾病是否会促进房颤的发展及其发生机制。本研究通过注射野百合碱形成PH大鼠模型,并在右室疾病形成后的21天对大鼠进行分析。野百合碱可以增高大鼠右室的压力和质量,右房也会增大。在32只PH大鼠中,有32只(100%)大鼠诱发了房颤,对照组的诱发率为6%(p < 0.001)。PH大鼠有明显的
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
52
#传导系统#
48
学习了
88
#ACC#
57