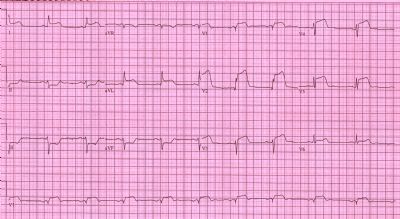
AHA/ACC更新STEMI患者直接PCI治疗指南
2015-10-27 大鹏 译 医学论坛网
近日,美国心脏学会/美国心脏病学会(AHA/ACC)公布了最新的ST段抬高型心肌梗死(STEMI)患者直接经皮冠状动脉介入治疗(PCI)指南修改意见【点此可下载英文原文】。全文发表于《美国心脏病学会杂志》(Journal of the American College of Cardiology)。指南集中修改的地方主要有两处,以下为与旧指南对比的更新建议。 一、罪犯血管——单一病变vs多支
近日,美国心脏学会/美国心脏病学会(AHA/ACC)公布了最新的ST段抬高型心肌梗死(STEMI)患者直接经皮冠状动脉介入治疗(PCI)指南修改意见【点此可下载英文原文】。全文发表于《美国心脏病学会杂志》(Journal of the American College of Cardiology)。指南集中修改的地方主要有两处,以下为与旧指南对比的更新建议。
一、罪犯血管——单一病变vs多支病变
|
2013年指南内容 |
2015年修订后指南内容 |
变化 |
|
若STEMI患者血流动力学稳定,不推荐直接PCI手术在非梗死相关动脉进行相关干预(推荐级别Ⅲ,证据等级B)。 |
对于存在多支病变且血流动力学稳定的特定STEMI患者,无论直接PCI或计划手术阶段,均可考虑在非梗死相关动脉进行PCI治疗(推荐级别Ⅱb,证据等级B-R)。 |
将推荐级别Ⅲ上调至Ⅱb,同时新指南放宽了手术时间窗选择,并纳入了多支病变。 |
二、血栓抽吸
|
2013年指南内容 |
2015年修订后指南内容 |
变化 |
|
直接PCI可考虑手动血栓抽吸治疗(推荐级别Ⅱa,证据等级B)。 |
1.在接受直接PCI治疗的患者群体,择期血栓抽吸与急救血栓抽吸的有效性尚缺乏足够的证据(推荐级别Ⅱb,证据等级C-LD)。 2.直接PCI前常规血栓抽吸无效(推荐级别Ⅲ,证据等级A)。 |
微调择期血栓抽吸与急救血栓抽吸的推荐等级,并加入了一项新的推荐,否定了直接PCI前常规血栓抽吸这一治疗方案。 |
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









不错的指南,为我们探讨研究提供了方针,给点个赞了!
46
很好,不错的指南资料,值得拥有值得收藏,值得探究。给自己学习探究提供方便。点个赞!
53
很好,不错的指南资料,值得拥有值得收藏,值得探究。给自己学习探究提供方便。点个赞!
51
#STEMI患者#
29
继续学习
56
继续关注
45
学习了讴歌了
52
#治疗指南#
23
#直接PCI#
30
可以
80