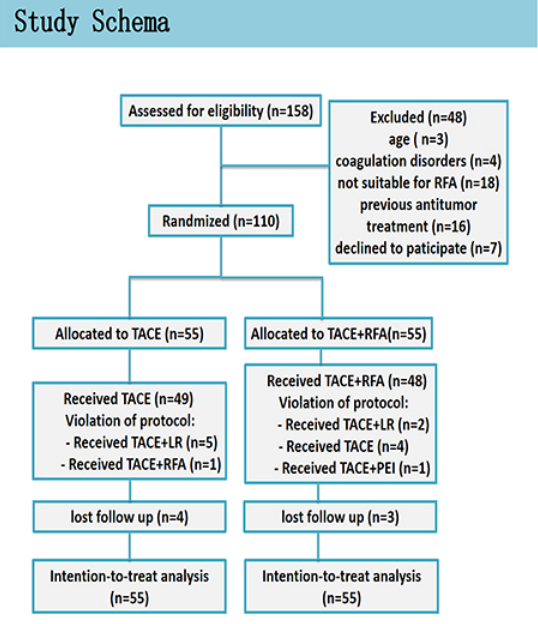
ASCO2019|TACE + RFA联用治疗中期(BCLC B期)肝癌改善患者生存期
2019-06-04 小M MedSci原创
第55届美国临床肿瘤学会(ASCO)年会于2019年5月31日至6月4日在美国芝加哥召开。本次会议吸引世界3万8千名肿瘤专家参与。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#患者生存#
42
#ACE#
29
#联用治疗#
28
#ASC#
37
#TAC#
31
#生存期#
33
肝癌,接下来就要细分了,对于体质好的病人,能否将PD-1类+抗血管新生+放疗等相结合,甚至有必要用TACE进行减负
34