Crit Care:重症心脏超声进展
2018-04-04 惠夏 重症医学
重症医师使用重症心超(CCE)技术,对急性心肺衰竭患者进行床旁诊疗。出于规范化教育的要求、对血流动力学监测工具的替代、以及持续技术进步,CCE越来越被认为是一种对重症患者无可比拟的血流动力学评估技术。表1中列出了CCE这一活跃领域中的最新研究进展。
重症医师使用重症心超(CCE)技术,对急性心肺衰竭患者进行床旁诊疗。出于规范化教育的要求、对血流动力学监测工具的替代、以及持续技术进步,CCE越来越被认为是一种对重症患者无可比拟的血流动力学评估技术。表1中列出了CCE这一活跃领域中的最新研究进展。
CCE可以为休克患者提供独特的形态学和功能学信息,并实时描述血流动力学特征。近期欧洲重症学会的循环休克与血流动力学监测共识中推荐使用CCE作为判断休克类型的初始手段,而非其他有创技术。为了提供充分的培训,国际圆桌会议最近介绍了所应掌握的理论知识和实践技能,以便重症医师能够具备基础和进阶CCE技术。所有重症医师都应接受基础CCE的初级培训。而进阶CCE需要更广更深入地训练,可以作为能力培养的可选部分来实施。使用电脑模拟系统可以加快经食道超声心动图(TEE)评估危重患者血流动力学的学习曲线。
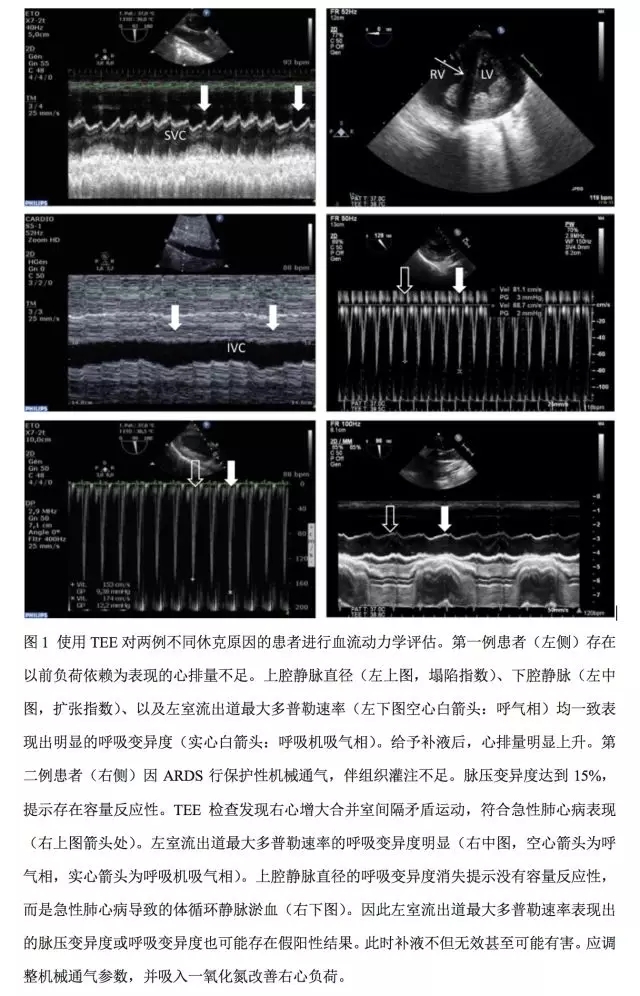
CCE有助于评估患者的容量反应性,以及各种呼吸条件下休克患者扩容的有效性和耐受性。近期一项多中心前瞻性研究观察了540例合并休克的机械通气患者,使用被动抬腿试验(PLR)模拟暂时性扩容,并行TEE监测。所有患者均可测得上腔静脉塌陷指数,另有78%的患者可获得其他用以预测容量反应性的动态指数。其中左室流出道多普勒最大速率是敏感性最高的参数,而上腔静脉塌陷指数的特异性最高。某些参数数据偏倚范围较大,研究者建议在补液高风险患者(如ARDS)中使用特异性较高的参数来精确评估容量反应性。另一种更灵活的方法是使用连续小剂量扩容的策略,并反复行CCE评估其有效性和耐受性。更重要的一点,CCE是唯一可以将脉压或每搏量(脉搏轮廓法)呼吸变异度与右心室联系起来的方法(图1),从而可避免容量反应性的假阳性诊断。
CCE在急性呼吸衰竭患者的诊疗中起重要作用。通过评估左心室舒张性能和灌注压力,CCE可准确地区分心源性肺水肿和撤机所致肺水肿,以及潜在的心肌病。根据ARDS柏林定义,推荐使用超声心动图来排除静水压性肺水肿。由于临床上急性肺心病的发生率可高达22%,有必要设计一项风险评分来区分出应接受CCE检查的患者。而TEE也可用于急性肺心病时潜在卵圆孔未闭的诊断。
无论是用于基础水平的聚焦心脏评估,还是作为进阶程度的复杂性血流动力学评估手段,CCE都能够为循环衰竭的诊疗提供可靠信息。将病理生理与临床结合,CCE有助于区分低血容量、左右心衰竭、填塞或其他原因所致的循环衰竭情况(图1)。CCE的另一个应用领域是用于复杂开放性心脏手术,以及接受高危循环辅助支持治疗患者的诊疗。
CCE可以精确测量心排量。因此常被用于评估被动抬腿试验或左心每搏量补液试验的有效性,以及对心脏灌注压诱发变化的耐受性。与其他血流动力学监测系统比较,CCE还可以提供其他临床相关信息。使用CCE和经肺热稀释法,对137例机械通气病例中37名存在感染性休克的患者分布进行独立评估。两种方法各自描述的血流动力学特征并不一致,其中有43%的发现来自CCE。事实上,大量血流动力学问题以及急性心脏/大血管病变仅能通过CCE来确诊,其中包括急性肺心病,左室流出道梗阻,重度瓣膜反流或狭窄,中央型解剖分流,重度肺栓塞及主动脉夹层。
电子技术的持续进步使小型化的超声设备成为可能。实时三维超声心动图以及基于斑点追踪的新型心肌功能定量测定方法可进一步提升CCE的诊断能力。与传统左室射血分数(EF)指标相比,利用斑点追踪测定感染性休克患者的整体左室长轴收缩期峰值应变来诊断脓毒性心肌病,其敏感性更高。后一指标在大部分EF下降的患者中同时出现异常。在部分延迟性左室收缩障碍的患者中,这一指标可先于EF出现下降。这一新指标能否用于预测左室收缩功能有待于进一步证实。
综上所述, CCE为一线重症医师对心肺疾病患者实施个体化紧急救治提供了广阔空间和新型血流动力学参数。无论操作者掌握的程度如何(基础、进阶或专家级)均可从中获益。而这些新近提出的基于超声心动图的治疗策略和新方法还需大样本重症病例来进一步验证。随着CCE日臻完善,美好时代即将到来。
表1. CCE新进展要点
1. 推荐CCE作为休克患者的一线评估方法。
2. 可根据不同的标准化教育需求进行基础或进阶CEE培训。
3. CCE可指导一线重症医师评估患者容量需求。
4. 推荐CCE用于ARDS诊断。
5. CCE诊断策略简单可靠。
6. 除作为诊断工具外,CCE用于监测设备更佳。
7. 持续技术改进提高CCE应用范围(斑点追踪技术)
8. CCE是不稳定患者个体化治疗的理想指导工具。
原始出处:
Philippe.What is new in critical care echocardiography?Crit Care. 2018; 22: 40.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#心脏超声#
42
学习了受益匪浅
58
好文献.学习了
0
很好.特别有用
55
学习了受益匪浅
46