Biomaterials:甲状旁腺激素可促进老年大鼠血管化骨再生和种植体骨整合
2018-07-04 MedSci MedSci原创
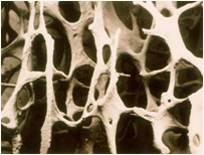
随着衰老而发生的骨量减少和成骨能力受损可影响牙种植体的结局。甲状旁腺激素(PTH)(1-34)是一种用于治疗骨质疏松症的合成代谢剂。然而,关于其在血管化骨再生和植入骨老化中的作用和机制知之甚少。在目前的研究中,我们采用体内和体外方法探索PTH(1-34)早期作用于血管生成和成骨微环境的机制,以增强老年大鼠的种植体骨整合。选取20个月龄的雌性大鼠,种植后次日开始每天皮下注射30μg/kg PTH(1
随着衰老而发生的骨量减少和成骨能力受损可影响牙种植体的结局。甲状旁腺激素(PTH)(1-34)是一种用于治疗骨质疏松症的合成代谢剂。然而,关于其在血管化骨再生和植入骨老化中的作用和机制知之甚少。在目前的研究中,我们采用体内和体外方法探索PTH(1-34)早期作用于血管生成和成骨微环境的机制,以增强老年大鼠的种植体骨整合。
选取20个月龄的雌性大鼠,种植后次日开始每天皮下注射30μg/kg PTH(1-34),持续5周。放射学和组织学分析证实,PTH(1-34)改善了老年大鼠早期的新骨形成,血管生成和种植体骨整合。老年骨髓间充质干细胞(BMSCs)的成骨潜能增强,而脂肪生成能力减弱。此外,在体外PTH(1-34)通过内皮细胞迁移和血管形成直接促进血管生成。同时,PTH(1-34)通过分泌血管生成和成骨生长因子刺激更多的破骨细胞参与骨重建,以诱导早期血管形成并间接刺激BMSCs的迁移或分化。
总之,这些结果揭示了PTH(1-34)调节血管生成和成骨微环境,从而导致更活跃的骨重建和新骨形成的机制,使其成为老年患者中快速血管化骨再生和植入物骨整合的潜在治疗剂。
原始出处:
Jiang L, Zhang W, et al., Early effects of parathyroid hormone on vascularized bone regeneration and implant osseointegration in aged rats. Biomaterials. 2018 Jun 26;179:15-28. doi: 10.1016/j.biomaterials.2018.06.035.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Biomaterials#
29
#血管化#
37
#Bio#
30
#种植#
35
学习一下.还不错
44
学习一下很不错
49
学习一下
49
#种植体#
25
#甲状旁腺#
24
#骨再生#
26