Circ Cardiovasc Inte:阜外医院颜红兵团队研究:TMAO可作为STEMI患者斑块破裂的新型生物标志物
2019-01-09 国际循环编辑部 国际循环
近日,中国医学科学院阜外医院颜红兵团队开展的一项最新研究在Circulation:Cardiovascular Interventions发表。既往报道发现,三甲胺N-氧化物(TMAO)可促进动脉粥样硬化的发病,与心血管事件风险相关,而血浆TMAO是否与急性心肌梗死患者的斑块形态相关尚不清楚。
近日,中国医学科学院阜外医院颜红兵团队开展的一项最新研究在Circulation:Cardiovascular Interventions发表。既往报道发现,三甲胺N-氧化物(TMAO)可促进动脉粥样硬化的发病,与心血管事件风险相关,而血浆TMAO是否与急性心肌梗死患者的斑块形态相关尚不清楚。颜红兵团队的这项研究探讨了ST段抬高型心肌梗死(STEMI)患者罪犯斑块形态与血浆TMAO浓度的关系。
图1.研究流程图
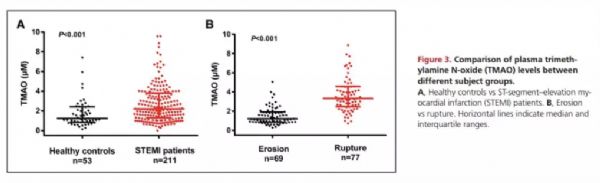
该前瞻性系列研究纳入211例STEMI患者,对罪犯病灶进行预干预光学相干断层扫描(OCT)检查;77例和69例患者分别被分类为斑块破裂组和斑块侵蚀组。使用稳定同位素稀释液相色谱串联质谱法检测血浆TMAO水平,斑块破裂患者明显高于斑块侵蚀患者(3.33μM;四分位数间距:2.48~4.57 vs.1.21μM;四分位数间距:0.86~1.91;P<0.001)。
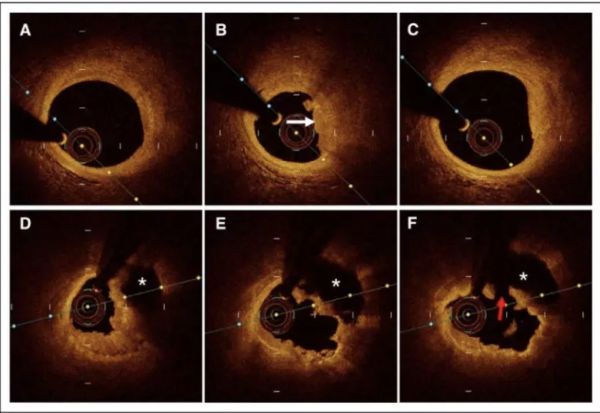
图2. 斑块侵蚀和破裂的代表性OCT图像
校正传统危险因素后,TMAO水平升高与斑块破裂独立相关(校正OR=4.06,95%CI:2.38~6.91;P<0.001)。斑块破裂与斑块侵蚀的受试者工作特征曲线下面积为0.89。在1.95μM界值水平下,TMAO在鉴别斑块破裂与斑块侵蚀方面具有88.3%的灵敏度和76.8%的特异性。
图3.不同组受试者间TMAO水平比较
上述研究结果提示,高水平的血浆TMAO与STEMI患者的斑块破裂独立相关。此外,TMAO可能是斑块破裂的有用生物标志物,可改善STEMI患者的危险分层和治疗。
颜红兵教授点评
OCT技术具有极高的分辨率,可识别罪犯斑块的病理类型。然而,临床应用中,OCT由于操作的有创性及费用高,难以在临床得到广泛应用。因此,寻找可替代的生物标志物早期发现急性心肌梗死患者的病理斑块类型,对患者的危险分层和治疗具有重要意义。
我们团队正在进行更大规模、更深入的相关研究,这项研究的意义在于,通过选择用新型生物标志物TMAO可以更早判断患者的斑块类型是斑块侵蚀还是斑块破裂,从而为未来临床实践中患者的风险分层和治疗提供一个更好的工具。
原始出处:
Yu Tan, Zhaoxue Sheng, Peng Zhou, et al. Plasma Trimethylamine N-Oxide as a Novel Biomarker for Plaque Rupture in Patients With ST-Segment–Elevation Myocardial Infarction. Circulation: Cardiovascular Interventions. Originally published 2 Jan 2019.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#标志物#
39
#斑块破裂#
30
#阜外医#
38
#ASC#
25
#STEMI患者#
45
#阜外医院#
30
#斑块#
29
#TMAO#
33
#STEM#
32
#生物标志#
23