CTS全国呼吸病学学术会议:李爱莉:心脏超声在CTEPH患者手术前后的心功能评价
2017-09-25 张竹 呼吸界
在中华医学会呼吸病学年会-2017第十八次全国呼吸病学学术会议上,中日医院李爱莉教授就“心脏超声在CTEPH患者手术前后的心功能评价”的主题做了演讲。现将演讲精华奉献给读者。
在中华医学会呼吸病学年会-2017第十八次全国呼吸病学学术会议上,中日医院李爱莉教授就“心脏超声在CTEPH患者手术前后的心功能评价”的主题做了演讲。现将演讲精华奉献给读者。
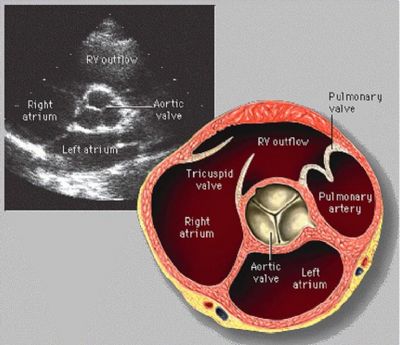
超声心动检查可以对CTEPH患者进行术前右心形态、血流动力学及右心功能状态的详细评估,协助病情判断,同时也可以除外是否合并其它基础疾病。作用不容忽视。
李爱莉教授首先对心脏超声评价右心功能的常用指标进行了介绍。包括传统指标:三尖瓣环收缩期纵向位移(TAPSE),右室心肌做功指数(RV IMP),右室面积变化分数(FAC)等。以及新指标:基于斑点追踪技术的右室游离壁纵向应变(RV GLS)和三维超声右室射血分数(RVEF)等。
CTEPH患者自身右心功能减低,代偿能力差,早期就会出现右心扩大、后负荷增加。肺血栓内膜剥脱术(PEA)术后,后负荷解除后,对于心脏超声有哪些指标可以用于术后疗效的评估目前并没有明确推荐。
以中日医院PEA术后病例为特点。患者术后肺动脉平均压及肺血管阻力明显下降。李爱莉教授团队对患者进行了长期随访,通过患者术前及术后70天超声心动图的对比提示,PEA术后患者右心大小、血流动力学及心功能有明显改善,但TAPSE及S’等指标在手术后无明显提高,常规指标中只有RV FAC可以反映右心功能的改善。新指标中RV GLS和3D RVEF对评价右心功能的改善可能更准确。
随后李爱莉教授又进行了相关内容的文献回顾,结果与中日医院团队前期数据统计结果相似。
最后,李爱莉教授指出:超声心动多项指标可用于CTEPH患者PEA术后右心功能的评估,有经验的中心可以通过测定RV GLS和三维RVEF更准确的评价PEA术后右心功能的改善情况。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#学术会议#
41
#呼吸病学#
40
厉害了
71
学习了
76
#呼吸病#
36
#评价#
32
#CTS#
40
#心功能#
34
#心脏超声#
44