Nat Commun:免疫监视细胞如何特赦有益细菌
2017-03-11 佚名 来宝网
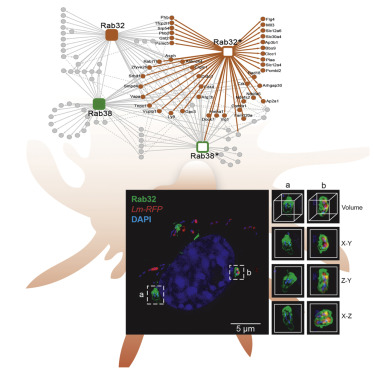
免疫系统的基本任务是其宿主(“自身”)和侵入性病原体(“非自身”)组织之间的辨别——区分。为了将其威力瞄准适当的目标,它必须能够区分朋友和敌人。这对与肠的上皮内层相关的免疫细胞提出了特别的挑战。它们暴露于肠道的天然微生物群之中,这些微生物群本身起重要的有益的生理作用。因此,免疫系统必须以某种有效的方式阻止攻击这些细菌,尽管它们不属于“自我”类别。德意志 - 意大利合作研究现在已经发现了一种有助于在
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
34
#COMMUN#
0
#视细胞#
40
学习了,好文章谢谢分享
66
很好的学习资料,谢谢了。
79
好东西,谢分享。
73
文章真好,值得分享
77
非常好的资料,学习了
54
签到学习了很多。
38
免疫监视,是否有望通过它来拯救肿瘤患者
34