J Endod:细菌感染时人牙髓细胞表达炎症及硬组织形成相关细胞标志物
2018-05-03 lishiting MedSci原创
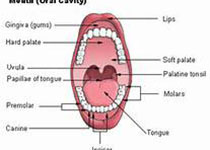
脂多糖(LPS)是引起深龋和牙髓炎时革兰阴性菌外膜的主要组成部分。当细菌侵入牙本质小管和牙本质持续受到损伤时,预先存在的成牙本质细胞会形成修复性牙本质。然而,LPS与修复性牙本质的关系还未可知。这篇研究的目的是为了评估LPS刺激是否会诱导人牙髓细胞(hDPCs)的硬组织形成。
脂多糖(LPS)是引起深龋和牙髓炎时革兰阴性菌外膜的主要组成部分。当细菌侵入牙本质小管和牙本质持续受到损伤时,预先存在的成牙本质细胞会形成修复性牙本质。然而,LPS与修复性牙本质的关系还未可知。这篇研究的目的是为了评估LPS刺激是否会诱导人牙髓细胞(hDPCs)的硬组织形成。研究培养永生化的dDPCs,将埃希氏菌来源的LPS (1 μg/mL)加入培养基中。在培养0, 1, 3, 7, 14和21天后获取样本,检测IL-1β, IL-6, Wnt5a, Runx2, ALP的信使RNA表达情况,并检测ALP活性。定量PCR结果显示,LPS组在刺激1天时IL-1β和IL-6的表达显著升高(P < .05)。14天时,LPS组的Wnt5a, Runx2和ALP的表达明显高于对照组(分别为2.0-, 4.7-和10.0-fold) (P < .01)。21天时,LPS组的ALP活性显著高于对照组(P < .01)。施加Wnt5a的抑制剂Box5,会减弱Runx2和ALP的表达(P < .05)。结论:这些结果表明,LPS刺激可以通过Wnt5a信号通路诱导hDPCs炎症
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#牙髓细胞#
22
#标志物#
31
#牙髓#
20
#细菌感染#
35
#髓细胞#
31