Nature:诺奖之后的新突破——大脑定位系统
2015-02-13 佚名 生物谷
2月11日,伦敦大学学院(UCL)的科学家在Nature杂志上发表研究论文,报道了其关于大脑网格细胞的新研究成果。大脑网格细胞的研究荣获2014年诺贝尔生理学及医学奖。而本研究的作者之一是恰恰2014年诺奖获得者之一的John O′Keefe教授。 本研究表明大脑的网格细胞能够通过周期性激发建立网络模式,形成具有局部环境的脑内地图,进一步作为动物的导航系统。然而,迄今为止,学界对于网格模式的认识
2月11日,伦敦大学学院(UCL)的科学家在Nature杂志上发表研究论文,报道了其关于大脑网格细胞的新研究成果。大脑网格细胞的研究荣获2014年诺贝尔生理学及医学奖。而本研究的作者之一是恰恰2014年诺奖获得者之一的John O′Keefe教授。
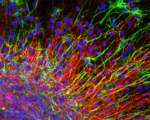
本研究表明大脑的网格细胞能够通过周期性激发建立网络模式,形成具有局部环境的脑内地图,进一步作为动物的导航系统。然而,迄今为止,学界对于网格模式的认识还是普遍认为其是六边形,为大脑提供均匀间隔以便测量距离。而这项新研究颠覆了之处在于,研究发现,网格模式会发生扭曲,以更好地匹配局部环境的几何形状,这意味网格之间的距离是可以发生变化的。
研究人员让41只大鼠在圆形、方形或梯形的环境中自由觅食,并检测其大脑内嗅皮层生成的网格模式。结果显示,网格模式是会依据环境形状改变的,在梯形环境中,六边形网格模式将被打破。研究人员进一步探索网格模式发生改变的原因,发现这种改变与环境的几何结构有关。
关于大脑的研究从来都是热点,手提微型电脑的发明者Jeff Hawkins也对大脑的研究深感兴趣,他建议将大脑看成一个记忆体,用于贮存和重演经历来有智慧地预计将会发生的事情(相关阅读,请点击:Jeff Hawkins:大脑研究将改变计算机科学)。相关的学者也在早前对于大脑地图进行过相关的报告,如脑科专家艾伦·琼斯在其演讲中展示了他的团队如何绘制每一个小区域里开启的基因,并且展示了他们之间怎样相互连接。(观看视频请点击:艾伦·琼斯:大脑的地图)
然而,网格模式为什么会根据环境发生改变?而且这对于网格细胞的导航作用的意义是什么?这些都还需要进一步的研究。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
26
#新突破#
27
小编评论亮了
165
perfect
64
#诺奖#
29