Diabetes:运动拯救精子!哈佛科学家发现运动能逆转高脂饮食对精子的有害影响,降低后代患肥胖和糖尿病的风险
2018-12-04 奇点糕 奇点网
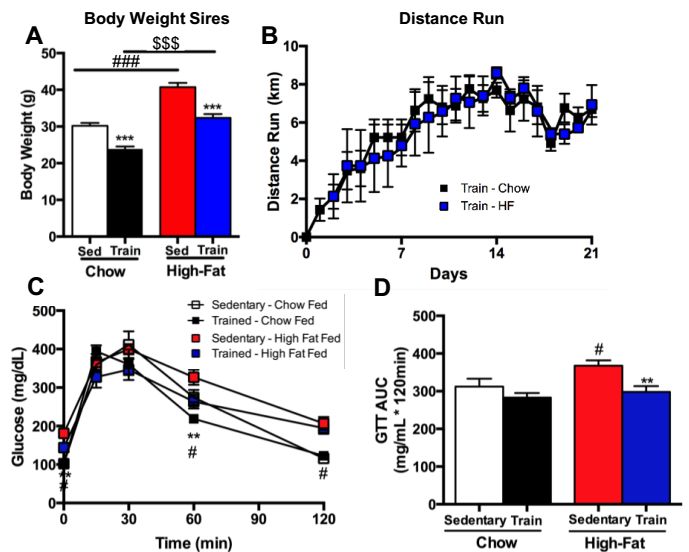
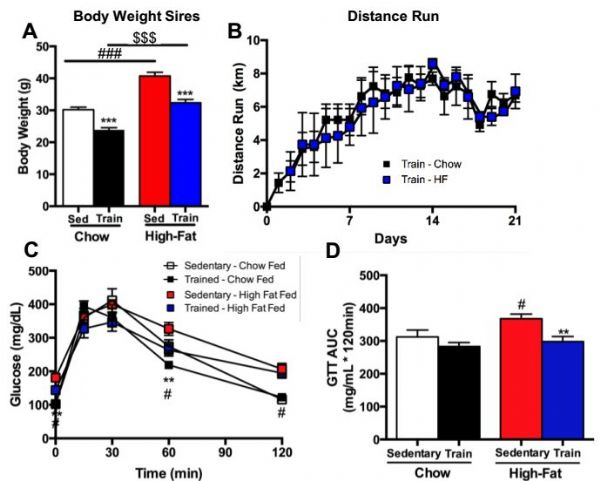
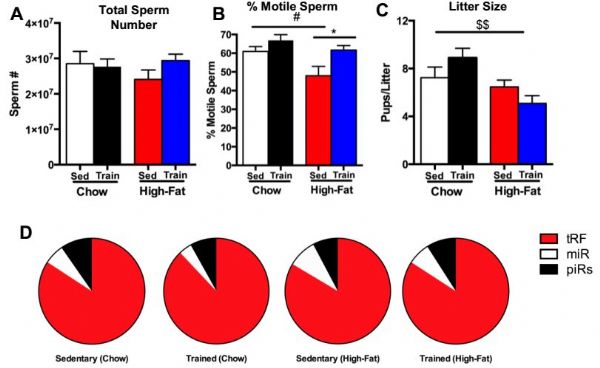
最近,美国哈佛医学院Laurie Goodyear和俄亥俄州立大学的Kristin Stanford博士在小鼠中发现,运动逆转了父亲因高脂饮食对精子造成的不良影响,从而改善了后代的葡萄糖代谢缺陷。这有助于减少后代的肥胖和2型糖尿病风险。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#科学家发现#
33
#DIA#
26
#BET#
37
#Diabetes#
25
#哈佛#
33
#高脂#
30
谢谢MedSci提供最新的资讯
0