Nano Letters:抗肿瘤纳米药物新成果----“变身”式纳米设计策略
2017-04-26 佚名 X-MOL
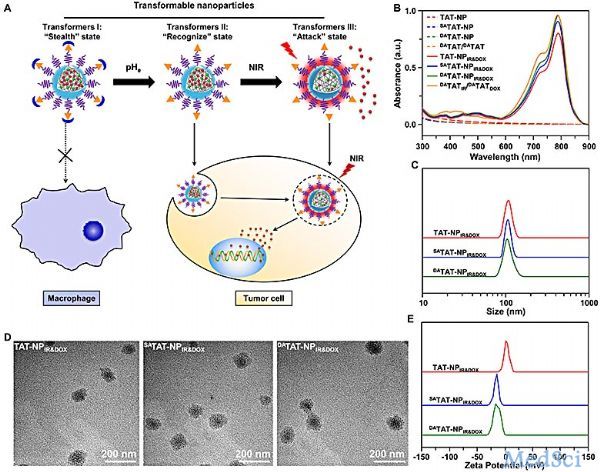
近日,华南理工大学医学院、生命科学研究院杨显珠教授及王均教授团队发展了一种“变身”式纳米策略,实现更精准、可控式抗肿瘤药物递送,研究成果发表在国际著名学术期刊 Nano Letters 上。抗肿瘤纳米药物通过静脉给药后,将会与生物系统(如其中的蛋白、细胞、体液、组织和器官等)进行复杂相互作用(nano-bio相互作用),这将极大程度地影响纳米药物的抗肿瘤效应。理想的抗肿瘤纳米材料进入机体后,能随着
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#TTE#
31
#新成果#
26
#ERS#
25
#纳米药#
44
和我想的有一点相似
56
#纳米药物#
27