CA-Cancer J Clin:罕见癌症的发病率增加!
2017-05-22 sunshine2015 来宝网
根据美国癌症协会的一份报告,在美国,大约五分之一的癌症诊断是罕见的癌症。该报告发表在CA:一份美国癌症协会的同行评审期刊上,该报告指出,罕见的癌症在儿童和青少年中发生的三种癌症中有超过两种。作者说,随着使用分子标记来对癌症进行分类,罕见癌症的比例可能会增加。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CA-Cancer#
29
#发病率#
29
学习了
44
学习
41
#罕见#
18
学习了
48
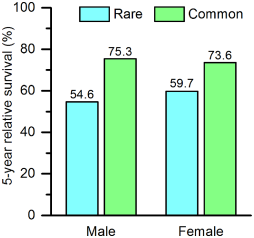
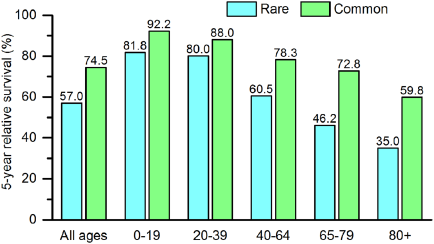
部分原因是由于这个阶段的分,5年相对生存率较低的患者相对于那些在男性(55%和75%)和女性(60%和74%)中被诊断为普通癌症的患者来说是比较贫穷的。 翻译貌似有些问题,没太看懂
46
学习了学习了
41
学习了谢谢分享。
25
文章很好,值得分享!
18