Eur Radiol:关于基于年龄和性别的急性胸痛患者行心脏CT血管造影的检查率和花费。
2017-09-20 shaosai MedSci原创
心绞痛是指由于冠状动脉粥样硬化狭窄导致冠状动脉供血不足,心肌暂时缺血与缺氧所引起的以心前区疼痛为主要临床表现的一组综合征。冠心病目前在我国的发病率呈逐年上升趋势,严重危害着人民群众的健康和生活。所以普及宣传冠心病的知识,积极有效地防止冠心病是对于提高人民群众的健康是有重要意义的。本研究旨在验证两个大型随机诊断性试验中基于年龄和性别亚组的医疗资源使用率,并将结果发表在Eur Radiol上。
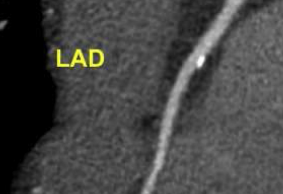
心绞痛是指由于冠状动脉粥样硬化狭窄导致冠状动脉供血不足,心肌暂时缺血与缺氧所引起的以心前区疼痛为主要临床表现的一组综合征。冠心病目前在我国的发病率呈逐年上升趋势,严重危害着人民群众的健康和生活。所以普及宣传冠心病的知识,积极有效地防止冠心病是对于提高人民群众的健康是有重要意义的。本研究旨在验证两个大型随机诊断性试验中基于年龄和性别亚组的医疗资源使用率,并将结果发表在Eur Radiol上。本研究汇集了来自ACRIN-PA 4005和ROMICAT II试验中的患者特异性数据。受试者随机分成标准治疗流程和使用心脏CT血管造影检查,并在入院时和1个月随访中记录急性冠脉综合征(ACS)的发生率和医疗资源使用情况。研究节点包括利用CCTA检出ACS和医疗资源利用情况。在行CCTA的1240例患者中,CCTA排除ACS的阴性预测值保持较高(≥99.4%)。进行额外诊断测试和花费比例随着年龄升高;与>60岁的女性相比,男性要高于女性(43.1% vs. 23.4%;$4559±3382 vs. $3179±2562, p<0.01)。男性用在排除ACS的花费较高,在>60岁以上的
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#心脏CT#
26
文章很好.值得分享
74
#造影#
29
很好的观点!
72
学习啦!谢谢分享!
80
学习了.谢谢分享
71
学习了受益匪浅
91
急性胸痛.需综合分析.选择检查.鉴别诊断.
27
好好努力学习
25