The Lancet Oncology:曲妥珠单抗不能提高HER2阳性晚期胃癌患者的生存率
2017-03-24 MedSci MedSci原创
曲妥珠单抗对既往接受过治疗的HER2阳性的局部晚期或转移性胃癌或食管胃交界腺癌无效
曲妥珠单抗联合化疗是治疗HER2阳性进展期胃癌的一线标准,但尚无有效的二线治疗方法。
研究人员考察了曲妥珠单抗对HER2阳性晚期胃癌治疗的患者(不能手术切除的、局部晚期,或转移性胃癌,包括胃食管交界处的腺癌)的耐受性和疗效。与紫杉醇相比未表现出明显的优势,该结果发表于近日的The Lancet Oncology。
在一项名为GATSBY的II/III期临床试验中,HER2阳性晚期胃癌或一线治疗后复发的患者被招募。试验的第一个阶段,患者随机分配接受曲妥珠单抗(n= 70,3.6 mg/kg 每三周或 2.4 mg/kg每周)或静脉滴注紫杉醇类药物(n= 75, 75mg/m2 多西他赛,每三周一次或者n=37, 80mg/m2 紫杉醇, 每周一次);在第二阶段,患者随机分配接受曲妥珠单抗(n=153,2.4 mg/kg 每周)或者静脉滴注紫杉醇类药物(n=80,剂量同前),试验的主要临床终点是患者的生存率(OS)。
试验结果显示,2.4mg/kg曲妥珠单抗组中位随访时间为17.5个月,紫杉醇组为15.4个月;2.4mg/kg曲妥珠单抗组中位生存期为7.9个月(95% CI 6.7-9.5),紫杉醇组为8.6个月(95% CI 7.1-11.2);2.4mg/kg曲妥珠单抗组发生三级或以上不良事件的概率要低于紫杉醇组(60% vs 70%);致死性不良事件、严重的不良事件以及导致治疗中断的不良事件发生概率两者相近;2.4mg/kg曲妥珠单抗组最常见的三级或以上不良事件为重度贫血(26%)、血小板减少(11%),紫杉醇组为白细胞减少症(39%)、重度贫血(18%);2.4mg/kg曲妥珠单抗组最常见严重不良事件为贫血、上消化道出血、肺炎、胃肠道出血,紫杉醇组为肺炎、中性粒细胞减少、白细胞减少。
相比于紫杉醇,曲妥珠单抗对于HER2阳性晚期胃癌患者的治疗未表现出明显的优势,对于HER2阳性的晚期胃癌患者现有的治疗手段仍很有限。
原文出处:
Peter C Thuss-Patience, MD, Manish A Shah et al. Trastuzumab emtansine versus taxane use for previously treated HER2-positive locally advanced or metastatic gastric or gastro-oesophageal junction adenocarcinoma (GATSBY): an international randomised, open-label, adaptive, phase 2/3 study. The Lancet Oncology. 2017 Mar 23.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
25
#曲妥珠#
32
#Oncology#
28
#胃癌患者#
18
#Lancet#
21
学习了!很受益!
61
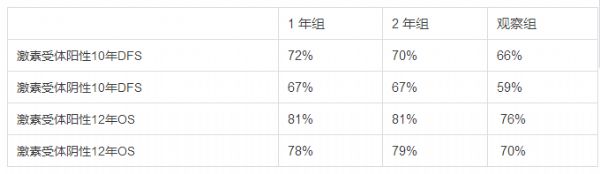
在乳腺有用啊
54
感谢分享一下!
47
谢谢分享,学习了。
56
#生存率#
16