Lancet Oncol:放疗与PD-L1抑制剂:携手共抗肺癌(KEYNOTE-001)
2017-05-31 王强 肿瘤资讯
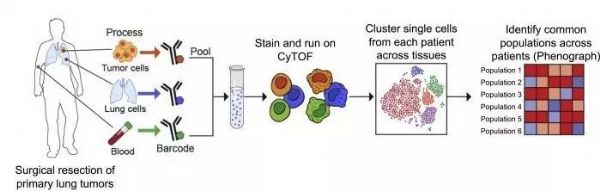
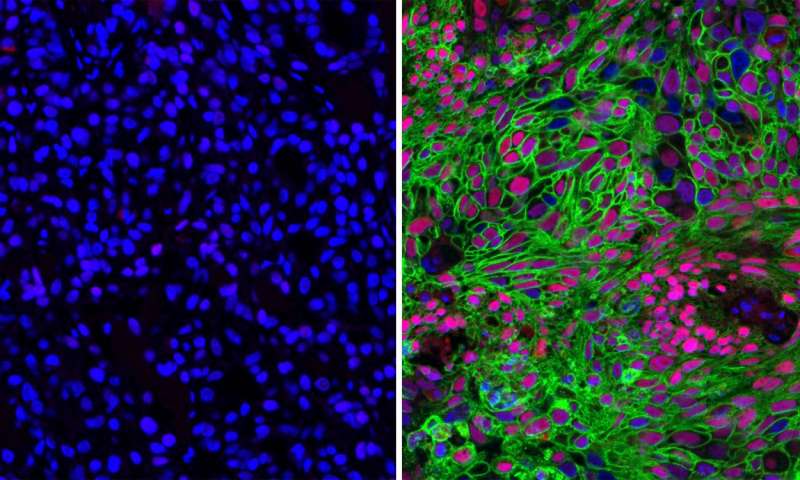
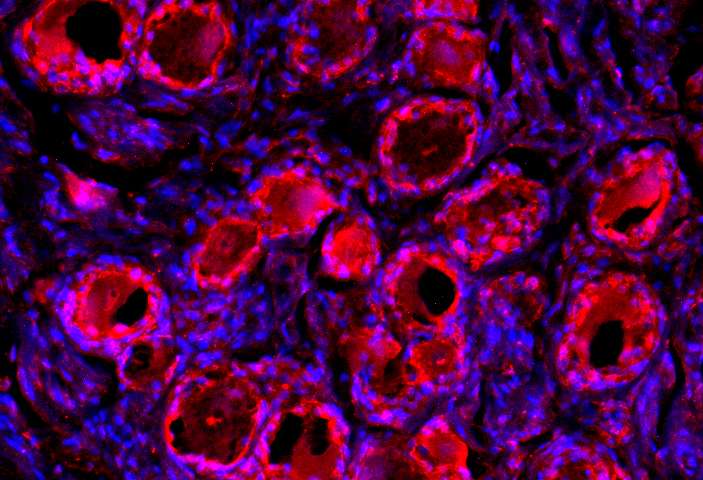
Lancet Oncology于5月23日在线发表了Shaverdian等人关于放疗联合pembrolizumab用于非小细胞肺癌治疗临床I期试验相关分析的文章,并配发了鲁汶大学医院Ruysscher的述评。检查点抑制剂用于转移性非小细胞肺癌(NSCLC)的一线及二线治疗,可以显着改善患者的无进展生存、总生存及生活质量。同时早已明确放疗也会活化免疫系统中与免疫治疗耐药相关的关键部分。很多癌症细胞并
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PD-L1抑制剂#
32
#Lancet#
30
#抑制剂#
45
继续学习
54
#Oncol#
30
#KEYNOTE#
34
不错的方式,努力学习,刻苦专研,不断总结出来新经验。给点个赞!
47
#PD-L1#
29
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
0
涨知识了,谢谢分享
54