Nat Biothechnol:装上了迷你版PD-1抗体的CAR-T细胞,对抗实体瘤如鱼得水
2018-08-15 小博 医麦客
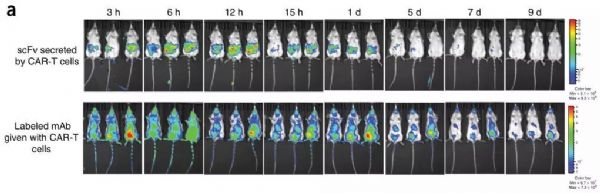
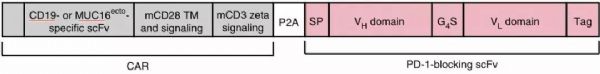
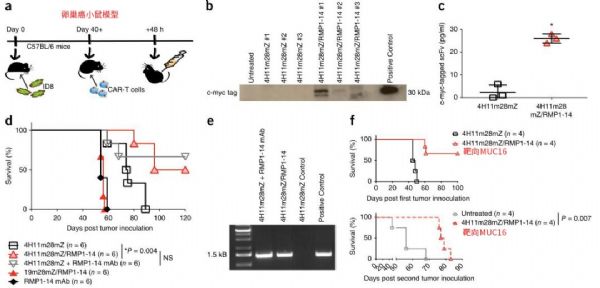
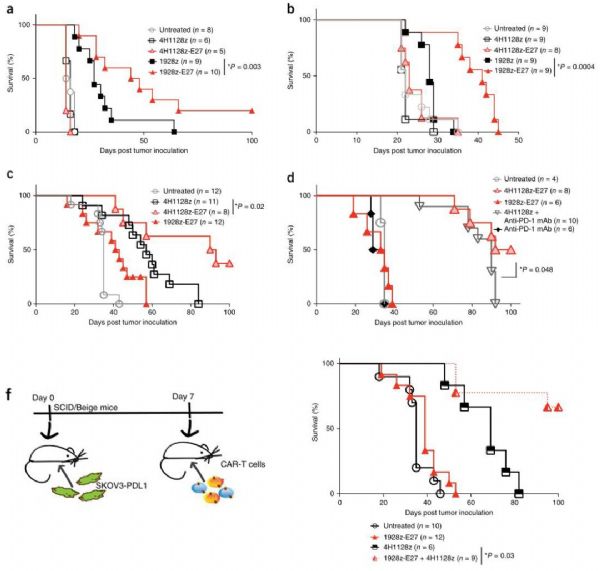
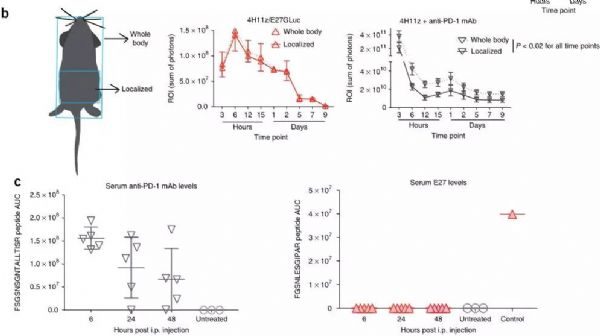
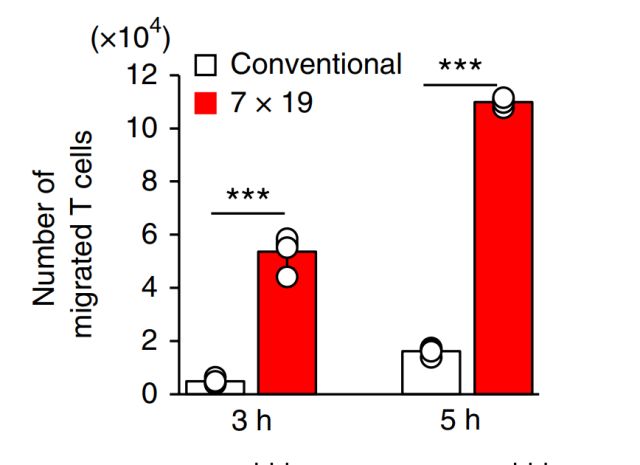
MSKCC(纪念斯隆凯特琳癌症中心)的科学家宣布他们已经建立了最新的工程化细胞,其具有强大的“装甲”战备,将两种最具潜力的免疫疗法——CAR-T细胞和检查点抑制剂组合在了一起,能够有效对抗实体瘤。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CAR-#
28
#Nat#
0
#Bio#
28
a:¥CnTwb1llNAq¥
59
#PD-1抗体#
32
感谢小编为我们准备了如此丰盛的精神大餐,同时也向作者致谢!认真学习了,点赞!
70
感觉很有希望,更高效,更小的副作用。
70