始基子宫合并阴道子宫内膜异位囊肿 1 例
2019-09-08 张炜悦 刘恩令 杨艳艳 现代妇产科进展
患者, 36 岁, G0P0,因“查体发现阴道壁肿物 1 个月”于 2017 年 11 月 1 日收入院。1 个月前患者查体时发现阴道前 壁尿道口下一直径约3+cm 肿物,囊性,无压痛,可活动,妇科 超声示:双侧残留子宫角? 为求进一步诊治遂就诊于我院。 2003 年患者( 22 岁) 被确诊为先天性无子宫,未予诊治,无明 显周期性腹痛。入院诊断:阴道壁肿物;先天性无子宫;原发 性闭经。入院查体:
1 病例简介
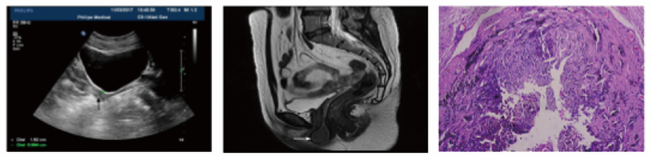
患者, 36 岁, G0P0,因“查体发现阴道壁肿物 1 个月”于 2017 年 11 月 1 日收入院。1 个月前患者查体时发现阴道前 壁尿道口下一直径约3+cm 肿物,囊性,无压痛,可活动,妇科 超声示:双侧残留子宫角? 为求进一步诊治遂就诊于我院。 2003 年患者( 22 岁) 被确诊为先天性无子宫,未予诊治,无明 显周期性腹痛。入院诊断:阴道壁肿物;先天性无子宫;原发 性闭经。入院查体: T 36.0℃, P 84 次/min, R 20 次/min, Bp 134/98mmHg;心肺未闻及异常,腹平软,全腹无压痛、反跳痛 及肌紧张,肝脾未触及肿大,叩鼓音,移动性浊音阴性,肠鸣 音正常存在。妇科检查: 外阴发育正常,尿道口下方阴道前壁可见约 3.5cm×3.0cm×3.0cm 大囊性肿物,无触痛及波动 感,无压痛,活动可,阴道通畅,顶为盲端,窥器可置入约 3cm,子宫缺如,双附件区未及异常。入院后完善相关化验检 查,卵巢功能正常。妇科超声示( 图 1A) : 始基子宫; 盆腔 MRI 结果回报( 图 1B) : 子宫未见确切显示,结合临床; 阴道 下段类圆形异常信号,考虑囊肿,囊内富含蛋白成份。2017 年 11 月 6 日行阴道壁肿物剥除术,台下切开囊肿,囊液为巧 克力样。术后予预防感染、止血、保护胃黏膜及补液治疗。 术后病理回报( 图 1C) :( 阴道前壁) 子宫内膜异位囊肿。术 后第 9 天患者痊愈出院,术后随访预后好。
图 1 B 超、 MRI 及术后病理图片 A:妇科彩超图像( 箭头示始基子宫) ; B: MRI 图像( 箭头示囊肿位置) ; C:术后病理( HE×100)
2 讨 论
始基子宫常无宫腔及宫内膜,症状为原发性闭经,无周 期性腹痛,第二性征发育良好,卵巢功能多正常,发病率约为 1/4000~1/5000 [1] 。子宫内膜异位症是激素依赖性疾病,形 态学上呈良性表现,但临床行为学上具有类似恶性肿瘤如种 植、侵袭及远处转移等特点。多种学说被提出来解释其发病 机制:经血逆流及淋巴血管转移、体腔上皮学说、遗传因素免 疫与炎症因素,以及近年提出的“在位内膜决定论”、“干细 胞学说”等。只有体腔上皮学说可解释无子宫及内膜结构的 子宫内膜异位症患者的发病原因。 始基子宫合并阴道子宫内膜异位囊肿,目前国内外报道 很少。Bricou 等[2]发现,子宫内膜在骨盆解剖结构中不对称 分布。Lazovic 等[3]报道 1 例 27 岁无子宫和卵巢的特纳综合 征患者,证实有子宫内膜出现。此类患者腹膜中,已证实残 留苗勒管组织可形成异位内膜组织的罕见情况[4]。Kourounis 等[5]表明,特纳综合征中,高度分化的上皮在不特定的刺激下可对子宫内膜腺体进行改造。Evelyn 等[6]报道, 1 例 20 岁子宫、宫颈、阴道及输卵管发育不全合并子宫内膜异位症。 以上病例均不能用经血逆流及植入学说来解释。19 世纪 Robert Meyer 提出的体腔上皮学说,认为苗勒管、卵巢表面上 皮、盆腔腹膜均由胚胎期具有高度化生潜能的体腔上皮分化 而来,在受到持续卵巢激素或慢性炎症反复刺激后,能被激 活转化成子宫内膜样组织; 而后提出的诱导学说认为,未分 化的腹膜组织在内源性生物化学因素诱导下可发展成子宫 内膜组织,种植的内膜还可诱导未分化的间充质形成子宫内 膜异位组织,该学说是体腔上皮化生学说的延伸,而在人类 尚无依据。除了体腔上皮化生,所有上述理论均依赖于子宫 结构和子宫内膜组织的存在。本例报道为子宫内膜异位症 的体腔上皮学说提供了临床上的支持,但其阴道前壁组织受 何种因子的刺激以及怎样生化成子宫内膜组织如何形成子 宫内膜异位症,仍需不断深化研究。
参考文献略。
原始出处:
张炜悦,刘恩令,杨艳艳,荆 楠等,始基子宫合并阴道子宫内膜异位囊肿 1 例报道并文献复习[J],现代妇产科进展,2019,28(9):719-720.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#子宫内膜异位#
25
#始基子宫#
27
#内膜#
31
#囊肿#
22