后纵隔海绵状血管瘤1例
2019-02-11 杨千朋 吴密侠 梁浩然 中国CT和MRI杂志
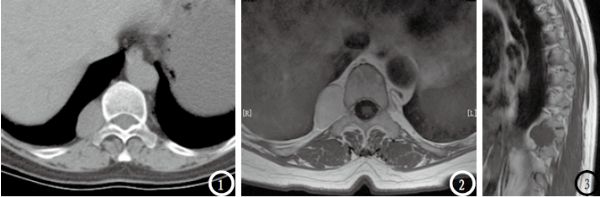
女,64岁。以“腰背部疼痛2月余”入院。患者无明显临床症状,查体示胸10水平压痛阳性。MRI平扫示胸10水平右侧脊柱旁沟团块状稍长T1长T2异常信号,境界清晰,信号均匀,大小约3.7 cm×2.3 cm×2.5 cm,邻近椎间孔略扩大;MRI增强示病灶中度均匀强化。
1.一般病例
女,64岁。以“腰背部疼痛2月余”入院。患者无明显临床症状,查体示胸10水平压痛阳性。MRI平扫示胸10水平右侧脊柱旁沟团块状稍长T1长T2异常信号,境界清晰,信号均匀,大小约3.7 cm×2.3 cm×2.5 cm,邻近椎间孔略扩大;MRI增强示病灶中度均匀强化。
CT平扫示病灶呈略低密度,CT值约27HU,密度均匀,境界光整。影像诊断:胸10水平右侧脊柱旁沟占位,考虑神经源性肿瘤可能性大。行胸腔镜下椎旁肿瘤切除术,术中见肿物位于第10胸椎脊柱旁沟内,质韧,与周围组织界限尚清。病理诊断:后纵隔海绵状血管瘤。
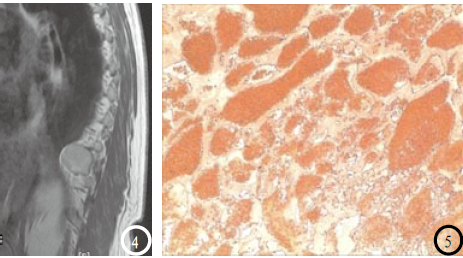
图1 CT平扫:胸10水平右侧脊柱旁沟椭圆形略低密度肿块,境界清晰,密度均匀。图3MRI平扫:病灶呈略低信号;图2、4MRI增强:病灶中度均匀强化,信号均匀。图5镜下(HE,×100):肿瘤由大小不等的薄壁血管构成。
2.讨论
纵隔海绵状血管瘤是一种比较罕见的纵隔血管源性肿瘤,占纵隔肿瘤的不足0.5%,好发生于前纵隔及后纵隔,中纵隔少见。肿瘤来源于被隔离的胚胎性血管母细胞组织或正常血管发育异常所致,由大小不一的海绵状血管窦构成,血管窦内可伴发静脉石。
本病好发于青壮年,性别差别不明显。多无明显临床症状,较大肿瘤可引起邻近组织器官的压迫症状。影像学表现多为类圆形、分叶状肿块,密度/信号均匀或不均匀,境界清晰,其内可见结节状、针尖状静脉石。静脉石的出现可作为本病的一个诊断标准。增强扫描与肿瘤的组织成分、血窦内血栓及血流有关,表现为不同的强化方式。本病例未发现静脉石是导致误诊的主要原因,再者由于对本病的认知不足,易与神经源性肿瘤相混淆。
总之,影像学表现境界清晰、密度/信号均匀或不均匀的肿块,应考虑到有海绵状血管瘤的可能,尤其是静脉石的出现。
原始出处:
杨千朋,吴密侠,梁浩然,张华文.后纵隔海绵状血管瘤1例[J].中国CT和MRI杂志,2018,16(02):151-152.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#后纵隔#
44
#血管瘤#
31
#海绵状血管瘤#
0
#海绵状#
44