Neurology:急性凸面蛛网膜下腔出血:一个未被认识的CAA-ri表现
2019-08-12 zyx整理 神经科病例撷英拾粹
非创伤性急性凸面蛛网膜下腔出血(cSAH)是脑淀粉样血管病(CAA)的常见表现,但在CAA相关炎症(CAA-ri)患者中罕有报道。
非创伤性急性凸面蛛网膜下腔出血(cSAH)是脑淀粉样血管病(CAA)的常见表现,但在CAA相关炎症(CAA-ri)患者中罕有报道。
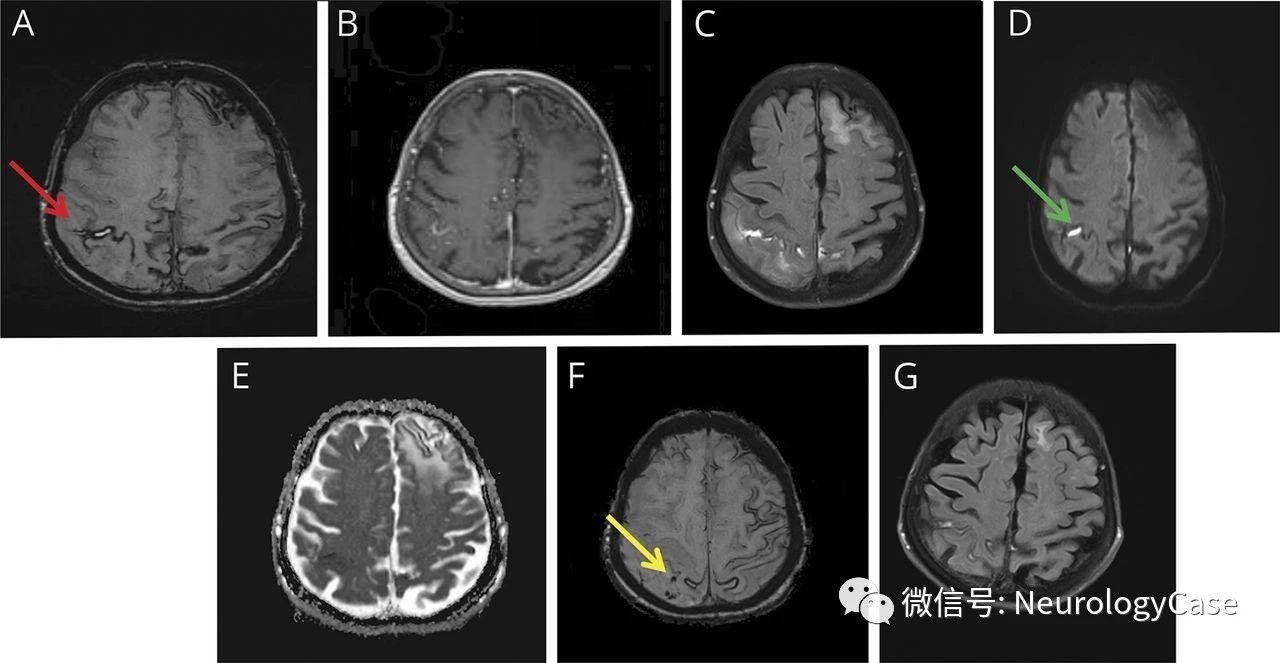
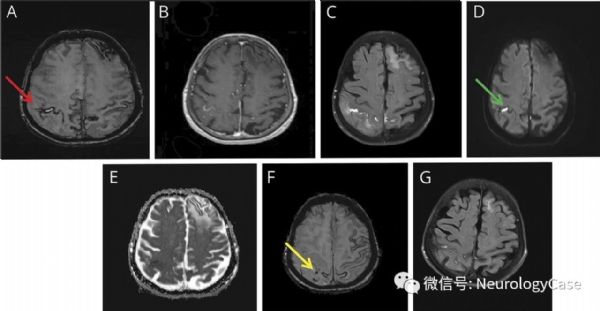
我们报道一例89岁女性的神经影像学表现,该患者有1个月的视幻觉,定向障碍和易激惹。脑MRI(图A-F)可见双侧半球播散性皮质表面含铁血黄素沉积,脑微出血和非对称性白质高信号。右侧顶叶还可见亚急性cSAH,伴蛛网膜下腔弥散受限和强化。
(图:磁敏度加权成像[SWI]可见凸面蛛网膜下腔出血[红箭,A];可见蛛网膜下腔强化[B]和FLAIR上不对称白质高信号[C];右侧顶叶弥散限制病灶[绿箭,D-E);SWI上亦可见脑皮质微出血[黄箭,F];皮质类固醇激素治疗后,右侧顶叶白质高信号消退[G])
原始出处:Theodorou A1, Lachanis S2, Alexopoulos P2, et al. Teaching NeuroImages: Acute convexity subarachnoid hemorrhage: An underrecognized presentation of CAA-ri. Neurology. 2019 Jul 30;
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#蛛网膜#
34
#CAA-ri#
26
#Neurol#
0
#CAA#
38