J Endod:人冻干牙本质基质可作为牙组织工程中的生物活性支架材料
2019-10-07 lishiting MedSci原创
牙本质是牙组织工程中适宜的支架材料,并且能为调节牙源性细胞提供适当浓度的生物活性蛋白成分。冻干是处理牙本质的一种可行策略,因其能够长效保持生物药剂产品以及牙本质的稳定,进而改善分布和存储。因此,作者认为:冻干牙本质基质(FDDM)能够为牙组织再生组成一种全新的生物结构支架。
牙本质是牙组织工程中适宜的支架材料,并且能为调节牙源性细胞提供适当浓度的生物活性蛋白成分。冻干是处理牙本质的一种可行策略,因其能够长效保持生物药剂产品以及牙本质的稳定,进而改善分布和存储。因此,作者认为:冻干牙本质基质(FDDM)能够为牙组织再生组成一种全新的生物结构支架。
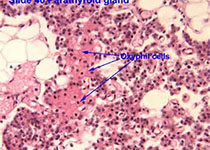
研究采用一种改良技术制备FDDM以保存牙本质的机械和生物特性。检测FDDM的抗压能力以及显微硬度。同时,检测其不同的生物特征,包括:细胞形态、细胞增殖、胶原分泌、碱性磷酸酶活性以及基因和蛋白表达。为了评估FDDM的体内诱导活性,将FDDM和人牙髓干细胞(DPSC)膜片同时植入裸鼠背部皮下。移植8周后,取出移植物并进行组织学观察和分析。
结果显示,FDDM的机械性能和生物学特点与牙本质相似(P > .05)。与培养于a-MEM或羟基磷灰石的DPSCs相比,培养于FDDM和牙本质上的DPSCs表现出极佳的细胞粘附、生长、活性和胶原分泌能力,但矿化能力减弱(P < .05)。组织学结果显示,FDDM与牙本质相似,支持体内牙本质/牙髓的组织再生,同时相关牙本质标志物表达水平上调,如:牙本质涎蛋白和碱性磷酸酶。
结论:这些结果表明,FDDM为牙组织再生构成了一种极佳的支架材料。
原始出处:
Wang F, Xie C, et al. Human Freeze-dried Dentin Matrix as a Biologically Active Scaffold for Tooth Tissue Engineering. J Endod. 2019 Sep 26. pii: S0099-2399(19)30589-8. doi: 10.1016/j.joen.2019.08.006.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#支架材料#
44
#基质#
35
#组织工程#
35
#牙本质#
23
学习了,谢谢分享
67