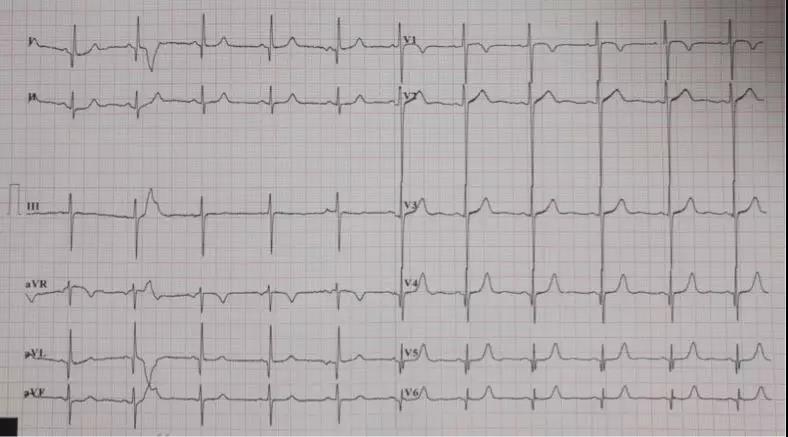
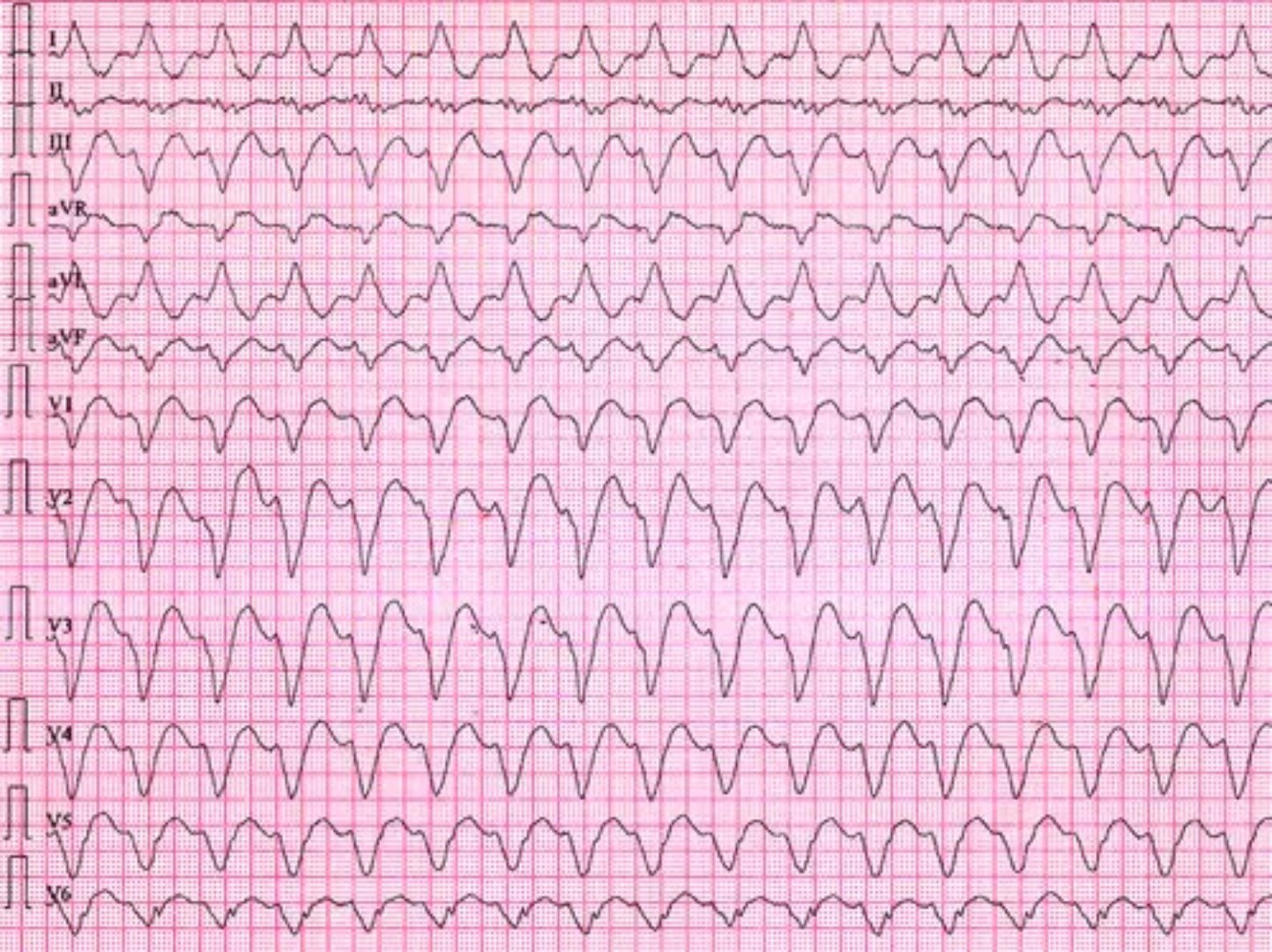
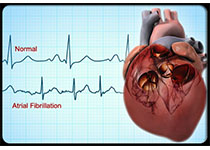
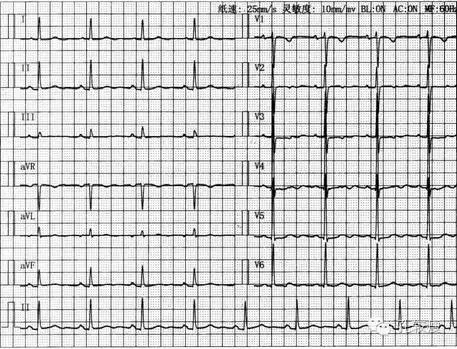
JAMA:美国预防工作组不建议用心电图筛查房颤:10秒“快照”没有比摸脉能发现更多房颤
2018-08-10 xujing 中国循环杂志
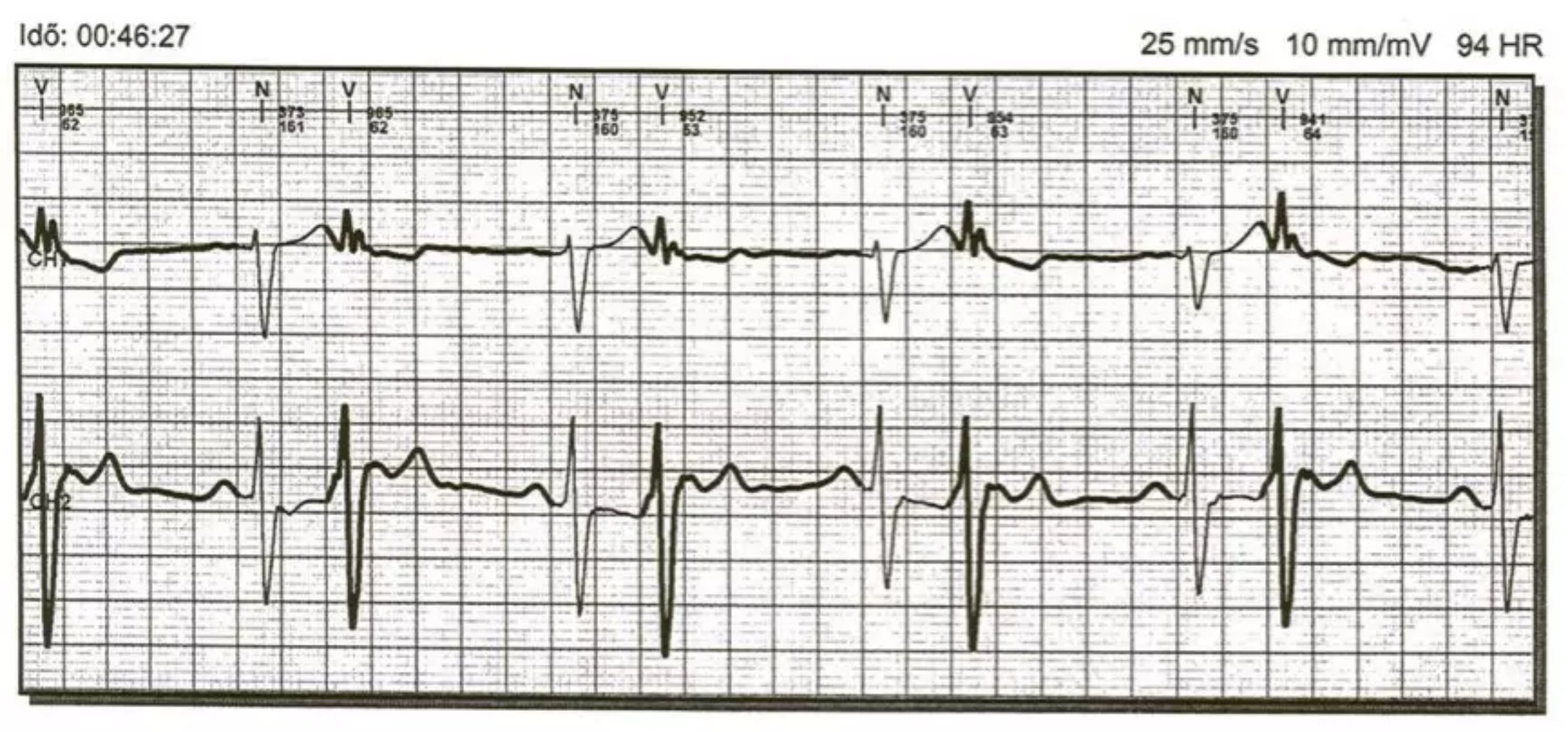
JAMA杂志近日刊登了美国预防工作组(USPSTF)声明。声明指出,采用心电图在无症状人群中进行房颤筛查的获益及风险不明确,证据不足。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#不建议#
0
哈哈,不错耶,学习了
41
#查房#
0
哈哈暴击
57