Clin Gastroenterology H: 肝硬化患者复发性腹水与死亡率的关系
2021-01-19 MedSci原创 MedSci原创
腹水是肝硬化最常见的并发症,10年内发病率约为60%。国际腹水联合会(ICA)根据两个主要标准对腹水进行分类:1)根据其数量和2)根据其对药物治疗的响应。
腹水是肝硬化最常见的并发症,10年内发病率约为60%。国际腹水联合会(ICA)根据两个主要标准对腹水进行分类:1)根据其数量和2)根据其对药物治疗的响应。腹水被分为三个不同的等级,根据腹内液体量:1级腹水只能通过超声波检查,2级腹水的特点是腹部中度对称扩张,3级腹水被定义为大或严重腹水与明显的腹部扩张。尽管有确切的定义,但对1级腹水或复发性腹水(即尽管饮食中存在钠限制和适当的利尿剂剂量,即使在12个月内至少3次复发的腹水)对患者预后的影响知之甚少。因此,本项研究旨在对此进行相关研究。

研究人员对2003年3月至2017年9月参加意大利护理管理计划研究的547名肝硬化门诊患者(259名无腹水,54名1级腹水,234名2级或3级腹水)的数据进行了事后分析。所有参与的受试者均被收集了人口统计学,临床和实验室数据,并且至少每6个月对患者进行了评估。如果可以的话,收集穿刺穿刺术的数量和体积。随访患者直至死亡,肝移植。中位随访时间为29个月。主要观察结果是死亡率和肝硬化并发症的发生。
研究结果显示存在1级与2级或3级肝硬化腹水患者的60个月无移植生存率无显着差异(36% VS 43%),但两组相比无腹水患者的生存率显着降低(68%; P<.001)。但是,具有1级腹水的患者的全身炎症等级和并发症发生率明显高于没有腹水的患者,但明显低于具有2级或3级腹水的患者。无腹水的患者与1级腹水之间的2级或3级腹水的发生率没有显着差异(10% VS 14%)。对药物有反应的腹水患者与复发性腹水的36个月无移植生存期无显着差异(78% VS 62%),而顽固性腹水的患者生存率明显低于有反应性或复发性腹水的患者。
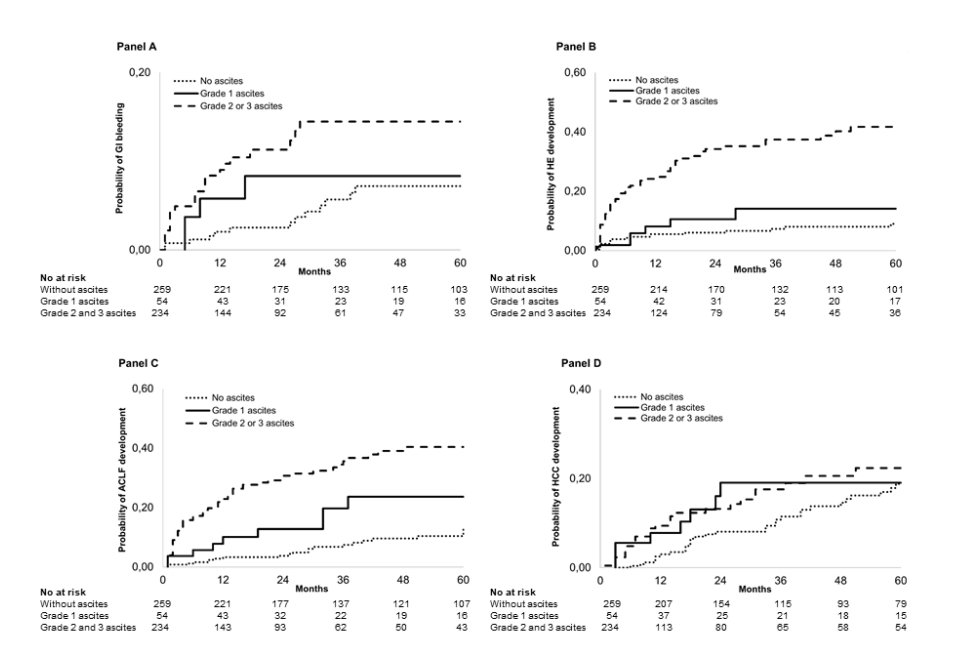
这项对来自大量肝硬化门诊患者的数据分析表明,研究人员发现,与无腹水相比,1级腹水与全身性炎症,更多的并发症和死亡率增加相关。复发性腹水患者与对药物有反应的腹水患者的死亡率无明显差异。
原始出处:
Marta Tonon. Et al. Outcomes and Mortality of Grade 1 Ascites and Recurrent Ascites in Patients With Cirrhosis. Clin Gastroenterology H.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#复发性#
33
#Gastroenterol#
0
#GAS#
51
#AST#
37
#Gastroenterology#
41
谢谢!最新的信息读起来就是收获大
50