JAMA Network Open:吸烟饮酒与多发性硬化有关
2022-04-19 影像小生 MedSci原创
高酒精摄入量与视网膜特征相关,表明有更严重的神经退行性变,而吸烟与被诊断为多发性硬化症的更高几率相关。
多发性硬化症(Multiple sclerosis, MS)是一种免疫介导的中枢神经系统脱髓鞘疾病,主要影响育龄妇女。遗传和环境因素都在MS的病理生理学中发挥重要作用。了解可改变的危险因素的作用,如吸烟、酒精摄入和肥胖,对指导临床咨询很重要。吸烟会增加患多发性硬化症的风险,建议患者戒烟以降低从临床孤立综合征(CIS)转化为多发性硬化症的风险是患者指导的一个重要部分。关于健康行为如何影响多发性硬化症患者的神经退行性变,我们所知甚少。脑容量的减少与更严重的残疾有关,特别是在认知领域。因此,改善神经退行性变已成为一个重要的治疗目标。
了解可改变的危险因素对多发性硬化症(MS)和相关神经退行性变风险的影响对指导临床咨询很重要。Iris Kleerekooper等在JAMA NETWORK OPEN杂志发表题为Associations of Alcohol Consumption and Smoking With Disease Risk and Neurodegeneration in Individuals With Multiple Sclerosis in the United Kingdom的研究文章,探讨饮酒、吸烟、肥胖与MS诊断及黄斑神经节细胞层和内丛状层(macular ganglion cell layer and inner plexiform layer, mGCIPL)厚度的关系。

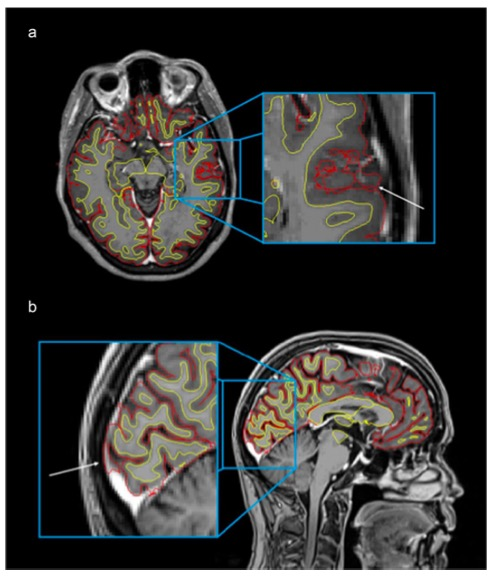
这项横断面研究分析了基于社区的英国生物库关于健康行为和视网膜厚度(通过双眼光学相干断层扫描测量)的研究数据,研究对象为40 - 69岁的人群。用多变量logistic回归分析确定危险因素。使用多变量广义估计方程来探讨饮酒和吸烟与mGCIPL厚度的关系。最后,使用交互作用模型探讨了酒精和吸烟与mGCIPL厚度的相关性在MS个体中是否存在差异。
共71981人(女性38685人[53.7%],男性33296人[46.3%];平均[SD]年龄,56.7[8.0]岁)纳入分析(20065名健康对照者,51737名有合并症的对照者,179名MS患者)。
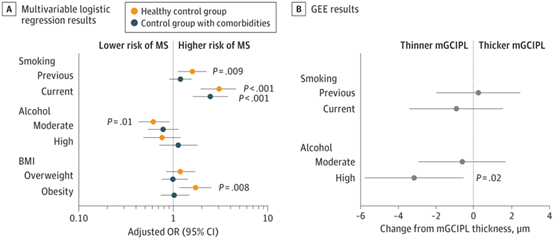
可改变的危险因素与多发性硬化症(MS)风险和黄斑神经节细胞和内丛状层(mGCIPL)厚度的可视化关联线状图
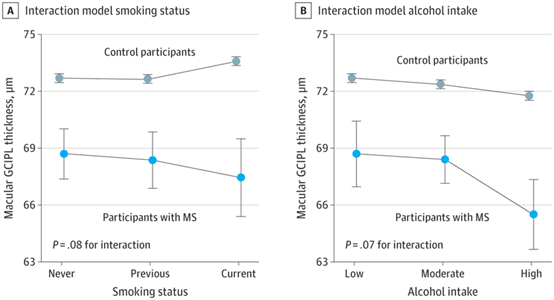
黄斑神经节细胞和内丛状层(mGCIPL)厚度与多发性硬化症(MS)诊断状况的相关性差异
1. 与MS病例状态显著相关的可改变危险因素为吸烟(比值比[OR]为3.05 [95% CI, 1.95-4.64])、适度饮酒(OR, 0.62 [95% CI, 0.43-0.91])和肥胖(OR, 1.72 [95% CI, 1.15-2.56])。
2. 与有合并症的对照组相比,只有吸烟与病例状态相关(OR, 2.30 [95% CI, 1.48-3.51])。
3. 在MS患者中,高酒精摄入与较薄的mGCIPL相关 (调整β =-3.09 [95% CI, -5.70至 - 0.48] μm;P = 0.02)。
4. 在酒精相互作用模型中,在对照组中,高酒精摄入量与较薄的mGCIPL相关(β = -0.93 [95% CI, -1.07至 - 0.79] μm;P<0.001),但与MS (β = -2.27 [95% CI, -4.76至 - 0.22] μm;P = 0.07)。在MS患者中,吸烟与mGCIPL厚度无关。然而,在对照组中,吸烟与较大的mGCIPL厚度相关(β = 0.89 [95% CI, 0.74-1.05 μm]; P < .001)。
这项横断研究发现,尽管适量饮酒与多发性硬化症的诊断几率较低有关,但大量饮酒与更明显的视网膜神经退化特征有关。吸烟与多发性硬化症的诊断几率增加有关。需要进一步的研究来确认这项研究的结果,特别是饮酒与多发性硬化症严重程度的复杂关联。研究结果表明,目前对普通人群的吸烟和适度饮酒的建议可能特别适用于被诊断为多发性硬化症或有患病风险的人。
原文出处
Kleerekooper I, Chua S, Foster PJ, et al. Associations of Alcohol Consumption and Smoking With Disease Risk and Neurodegeneration in Individuals With Multiple Sclerosis in the United Kingdom. JAMA Netw Open. 2022;5(3):e220902. doi:10.1001/jamanetworkopen.2022.0902
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#多发性#
33
#NET#
38
#PE#
31
感谢分享
44
JAMA上文章都是顶级的,谢谢梅斯及时上新
32