JACC:残余炎症可增加PCI术后患者不良心脑血管事件风险
2019-05-20 不详 MedSci原创
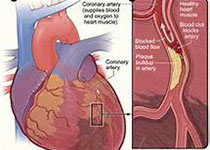
目前,对于残余炎症风险(RIR)对接受冠脉介入治疗(PCI)且基线低密度脂蛋白胆固醇(LDL-C)≤70mg/dl患者的影响尚不清楚。本研究的目的旨在评估PCI术后高RIR的发生率和影响。本研究纳入了2009-2016年基线LDL-C≤70mg/dl并进行了高敏C反应蛋白(hsCRP)评估的PCI患者,高RIR定义为hsCRP >2 mg/l。患者根据RIR状态分为持续性低RIR组、RIR减
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#脑血管事件##残余风险#
35
#血管事件#
32
#JACC#
42
#PCI术#
36
#ACC#
38
#PCI术后#
25
#心脑血管事件#
28