J Clin Oncol:R-CHOP方案+来那度胺可进一步改善新确诊DLBCL患者预后
2021-02-10 MedSci原创 MedSci原创
来那度胺联合R-CHOP(R2CHOP)可明显改善新确诊的DLBCL患者(包括ABC-DLBCL患者)的预后
来那度胺联合利妥昔单抗和环磷酰胺、阿霉素、长春新碱和强的松(R-CHOP)在未治疗过的弥漫性大B细胞淋巴瘤(DLBCL)患者中显示出了良好的疗效,尤其是对活化的B细胞样(ABC)亚型。东部合作肿瘤学小组(ECOG)-ACRIN试验E1412是一项随机的II期研究,比较了R2CHOP和R-CHOP在未治疗过的DLBCL中的疗效。
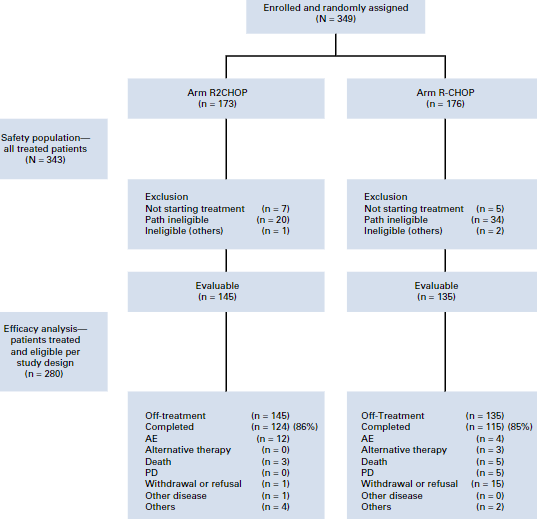
在该试验中,新确诊的国际预后指数(IPI)≥2、ECOG表现状态≤2分的II期大块型-IV期DLBCL患者随机分到R2CHOP组和R-CHOP组,共6个周期。主要终点是ABC-DLBCL患者的无进展生存期(PFS)。次要终点包括总缓解率(ORR)、完全缓解率(CR)和总存活率(OS)。
招募了349位患者,其中280位可纳入分析(R2CHOP组 145例,R-CHOP组 135例):ABC-DLBCL患者 94位、生发中心B细胞样DLBCL 122位、无法分型的 18位、不明确的 46例。
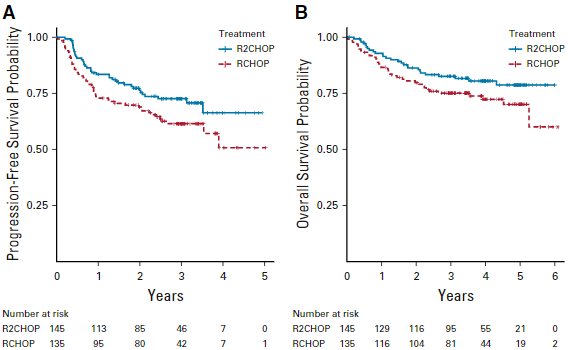
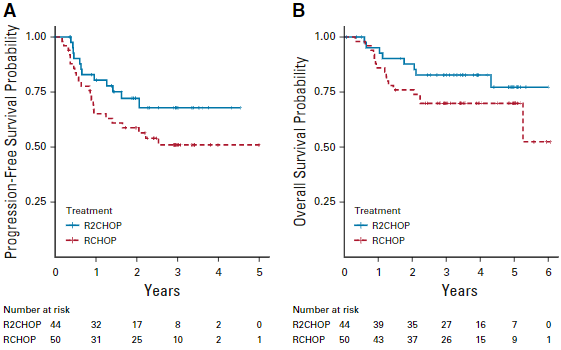
所有患者的PFS和OS
两组间的基线特征平衡良好,中位年龄 66岁(范围 24-92岁);70%的患者有IV期疾病;IPI得分为2、3和4/5的患者比例分别为34%、43%和24%。
骨髓抑制在R2CHOP组更为常见。R-CHOP组和R2CHOP组的ORR和CR率分别为92%和68% vs 97%(p=0.06)和73%(p=0.43)。
ABC-DLBCL患者的PFS和OS
中位随访 3.0年;与R-CHOP相比,R2CHOP组的疾病进展或死亡风险降低了34%(风险比[HR] 0.66,95%CI 0.43-1.01),3年PFS和OS均更高(PFS:73% vs 61%,p=0.03;OS:83% vs 75%,p=0.05)。
综上所述,该研究显示,来那度胺联合R-CHOP(R2CHOP)可明显改善新确诊的DLBCL患者(包括ABC-DLBCL患者)的预后。
原始出处:
Nowakowski Grzegorz S,Hong Fangxin,Scott David W et al. Addition of Lenalidomide to R-CHOP Improves Outcomes in Newly Diagnosed Diffuse Large B-Cell Lymphoma in a Randomized Phase II US Intergroup Study ECOG-ACRIN E1412. J Clin Oncol, 2021, undefined: JCO2001375.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#患者预后#
34
#LBCL#
53
#Oncol#
35
#J Clin Oncol#点击查看更多该期刊内容
76
涨知识
90
#DLBCL#
48
#R-CHOP#
47
#R-CHOP方案#
54
谢谢梅斯分享这么多精彩信息
71