JACC:经导管主动脉瓣置换术对右心室-肺动脉耦合的影响
2019-11-28 xiangting MedSci原创
TAVR对LV射血梗阻的直接缓解与RV功能和RV-PA耦合的改善有关。
这项研究目的是检验经导管主动脉瓣置换术(TAVR)的急性左心室(LV)卸载可以改善严重主动脉瓣狭窄患者(AS)右心室(RV)功能和RV-肺动脉(PA)耦合的假设。
RV功能障碍是TAVR患者预后不良的标志,这表明缓解阻塞对这类人群的益处较小。然而,LV和RV通过心室相互作用而相互影响,因而LV卸载会使RV功能改善。
症状性严重AS患者在TAVR前和之后进行前瞻性侵入性血流动力学评估,同时行超声心动图检查。
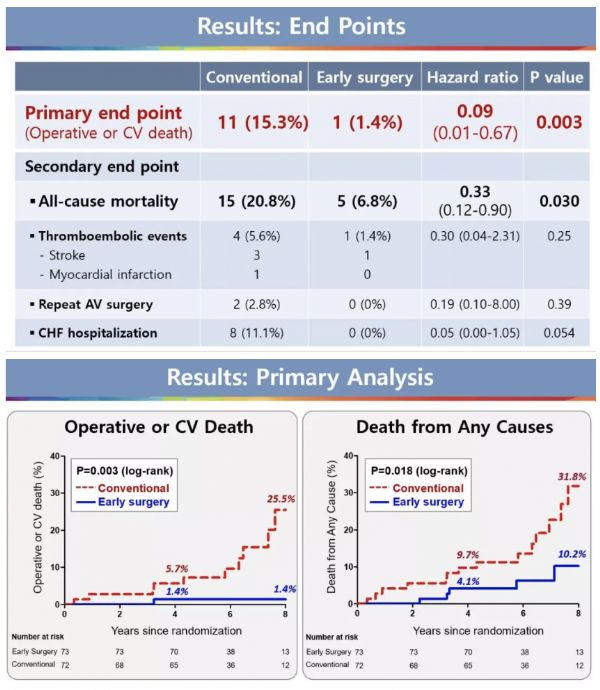
44例严重AS患者进行了TAVR(平均年龄81±8岁,女性占27%)。基线时,右心房、PA平均压(27±7mmHg)和肺毛细血管楔压(16±4mmHg)轻度升高,而正常心脏指数较低(2.3 l/min/m2)。肺血管阻力轻度升高(222±133 dynes ·s/cm5),PA顺应性轻度降低(3.4±1.4ml/mmHg)。TAVR后,主动脉瓣面积增加(从0.8±0.3到2.7±1.1cm2;p<0.001),平均主动脉梯度减低(从37±11到7±4mmHg;p<0.001),而心脏指数升高(2.3±0.5至2.5±0.6 l/min/m2; p=0.03)。LV每搏功、收缩末期壁应力和收缩射血期减少了23%至27%(p均<0.001),表明左室负荷明显减轻。RV每搏功(从16±7到18±7mmHg·ml;p=0.04)和三尖瓣环收缩速度升高(从9.5±2.0到10.4±3.5cm/s;p=0.01),同时PVR降低(194±113 dynes · s/cm5; p=0.03),表明RV-PA耦合得到改善。TAVR后RV每搏功增加与主动脉瓣面积增加的幅度直接相关(r=0.58;p<0.001)。
TAVR对LV射血梗阻的直接缓解与RV功能和RV-PA耦合的改善有关。这些发现为严重AS患者TAVR使得LV卸载对RV功能障碍的潜在益处提供了新见解。
原始出处:
Mackram
F. Eleid. Effect of Transcatheter Aortic Valve Replacement on Right
Ventricular–Pulmonary Artery Coupling. JACC:Cardiovascular Interventions. November 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#JACC#
35
#置换#
21
#ACC#
32
#主动脉瓣#
24
#主动脉瓣置换术#
24
#主动脉#
30
#经导管#
20
#经导管主动脉瓣置换#
33
#右心室#
28
#置换术#
27