Ann Palliat Med:自体软骨和硅胶假体隆鼻的疗效和并发症发生率有多大差别?
2022-07-01 医路坦克 MedSci原创
鼻整形术是一种整形外科手术,可以使用各种假体材料来雕刻或抬高鼻子以美化其形状,本文全面分析和比较了使用自体软骨(AC)和硅胶材料进行隆鼻手术的疗效和并发症发生率。
鼻整形术是一种整形外科手术,可以使用各种假体材料来雕刻或抬高鼻子以美化其形状,它是整形美容外科最常见的手术之一。传统的隆鼻手术是通过人工假体实现的,其材料包括硅胶、膨体聚四氟乙烯(ePTFE)和羟基磷灰石。
固体硅胶鼻假体是由高温硫化形成的固体聚合物,具有一定的弹性和硬度。有 "L "形和柳叶形固体硅胶假体,操作简单方便,价格相对低廉。此外,可以根据患者的鼻部雕塑制作个性化的假体,术后形态自然逼真。然而,固体硅胶置入部位存在变形和感染等并发症,研究统计,单纯使用硅胶假体(SP)的隆鼻手术并发症高达17%。
自体骨组织是另一种常用的隆鼻材料,其优点是移植后容易存活,无排斥反应;但也存在取材不便、长期骨吸收、形状改变等问题。
固体硅胶材料和自体软骨(AC)组织都有各自的优点和缺点。在这项荟萃分析中,我们全面分析和比较了使用AC和硅胶材料进行隆鼻手术的疗效和并发症发生率。
方法:通过关键词的快速匹配,检索Medline、Embase、PubMed、中国国家知识基础设施(CNKI)和万方等数据库,获得与AC隆鼻或硅胶填充隆鼻相关的随机对照试验,经筛选和质量评估后用Stata16.0软件进行分析。
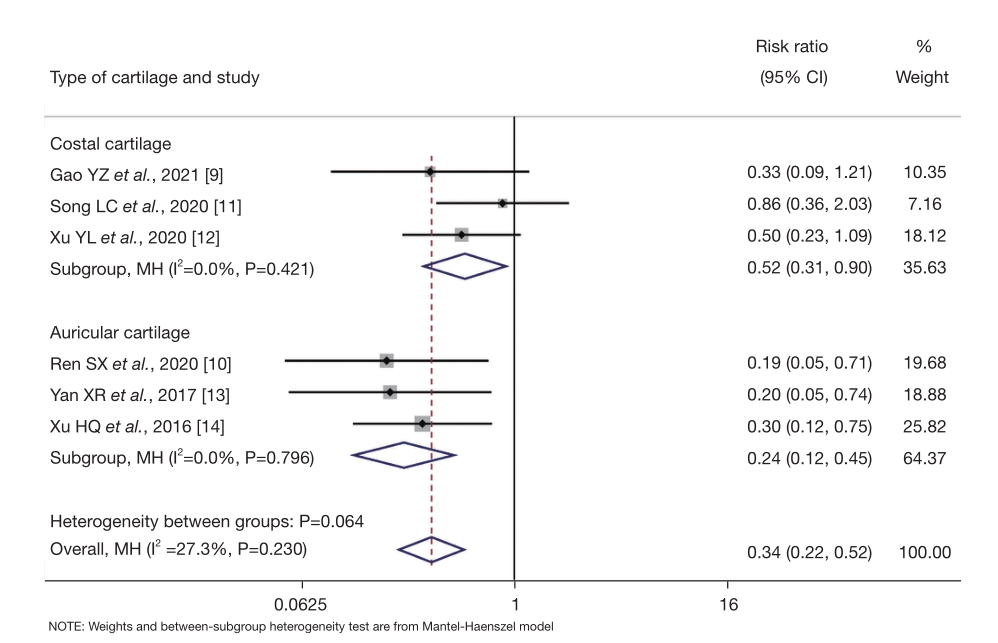
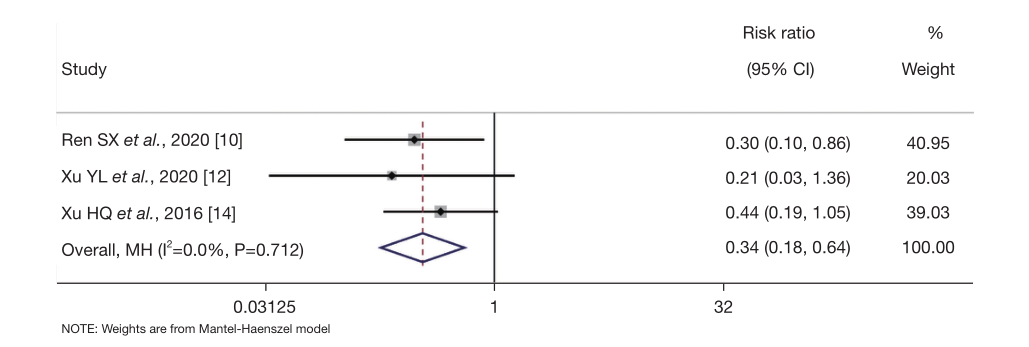
结果:本研究共纳入了7篇文章中的1233名接受隆鼻手术的患者。Meta分析显示,使用AC的隆鼻手术会获得更多的满意度[风险比(RR)=1.11;95%置信区间(CI):(1.02,1.21);Z=2.413;P=0.016]。 会降低并发症率[RR=0。 34; 95% CI: (0.22, 0.52); Z=-5.010; P<0.0001],与硅胶假体(SP)材料相比,二次手术率[RR =0.34; 95% CI: (0.18, 0.64); Z=-3.363; P=0.001]。
纳入文献的基本特征、参与者特征及质量评价得分

AC材料与SP材料的总体满意率比较。CI,置信区间

AC材料与SP材料鼻整形术的总体并发症发生率。CI,置信区间
AC材料与SP材料鼻成形术的二次手术率比较(10,12,14)。CI,置信区间
结论:在隆鼻手术中,使用AC材料可以获得更多的满意度,总的并发症率较低,而且二次手术率也比硅胶材料低。但基于研究中的异质性和发表偏倚,这一论点仍需通过纳入更多高质量的研究来进一步探讨。
文献来源:Wu C, Yang S, Zheng G, A systematic review and meta-analysis of the efficacy and complication rates of augmentation rhinoplasty with autologous cartilage and silicone prosthesis.Ann Palliat Med 2022 Mar;11(3)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#并发#
54
#发生率#
65
#ALL#
37
#假体#
49
#Med#
38