Clin Trans Gastroenterology:肝硬化患者难治性梭状芽胞杆菌感染的发病率和危险因素
2020-08-10 MedSci原创 MedSci原创
艰难梭菌(CDI)是一种常见的导致腹泻的微生物病原体,在门诊和住院患者中发病率和严重性都在增加。
艰难梭菌(CDI)是一种常见的导致腹泻的微生物病原体,在门诊和住院患者中发病率和严重性都在增加。尽管CDI检测和治疗取得了显着进步,但结果却继续恶化。常见的CDI危险因素包括住院,免疫抑制,晚期合并症以及使用抗生素和质子泵抑制剂等药物。这些危险因素在肝硬化患者中非常普遍,他们特别容易感染CDI,而且CDI也是死亡的独立危险因素,因此,我们试图确定肝硬化和CDI患者的危险因素及其相关结局。

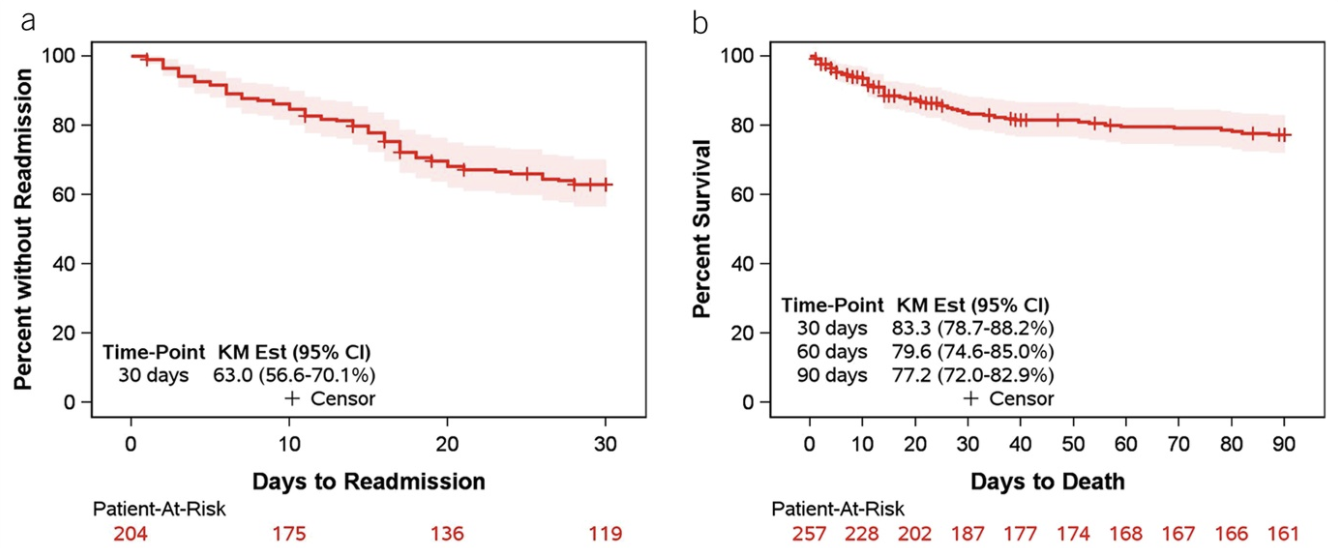
研究人员对2012年1月1日至2016年12月31日期间入住印第安纳大学医院的诊断为肝硬化的成年患者进行了一项回顾性队列研究,当患者诊断为CDI感染开始,对患者进行了90天的随访,以确定结果。主要观察结果是CDI的反复感染(R-CDI),其定义为在最初CDI诊断日期后14-56天内再次发生的CDI。与初始CDI的纳入标准一样,R-CDI的定义是基于相容的症状并伴有阳性实验室检查。次要结果包括CDI诊断90天内的死亡率和出院30天内的再次入院。使用Kaplan–Meier曲线统计R-CDI发生的天数。使用Cox比例风险模型评估患者特征与结果之间的单变量关联。
本项研究共纳入257位患者,其中有28位在2周内死亡,还有21位在2周后没有随访数据,剩下208位用于R-CDI分析。共有22例患者发生R-CDI,估计R-CDI发生率为11.9%。简单来说,R-CDI与年龄增加,非丙型肝炎肝硬化,查尔森合并症指数增加,住院时间增加有关。R-CDI与药物之间没有显着关联:出院时,有62%的患者正在服用质子泵抑制剂,含14.5%的R-CDI(相比之下,没有服用质子泵抑制剂的患者为7.6%;P= 0.15)。另外,有12%的人在放电时服用氟喹诺酮,R-CDI为21.8%(相比之下,不服用氟喹诺酮的则为10.7%;P = 0.18)。接受非达霉素治疗的患者和接受粪便微生物群移植的患者均发生CDI复发。另外,乳果糖的使用会增加R-CDI的风险(危险比[HR] 2.58; 95%置信区间[CI]:1.09–6.09)。在22例发生R-CDI的患者中,有9例(40.9%)符合严重CDI的标准,还有1例患有暴发性结肠炎。在这257名患者中,有53名在90天内死亡(入院时28例,出院后25例),死亡率为22.8%,在没有R-CDI的人群中,90天死亡率为20.8%。死亡与肝硬化的非酒精性脂肪性肝炎病因,严重的CDI,暴发的CDI,万古霉素治疗,Child-Pugh评分增加,MELD评分增加和重症监护有关。
本项研究通过较为仔细的随访发现肝硬化患者的R-CDI率为约为11.9%,年龄增加,非丙型肝炎肝硬化,查尔森合并症指数增加,住院时间增加是引起肝硬化患者患有CDI的主要原因,具有这些危险因素的患者尽早干预可以有效改善患者预后。
原始出处:
Phatharacharukul, Parkpoom. Et al. Incidence and Risk Factors of Recurrent Clostridioides difficile Infection in Patients With Cirrhosis. Clin Trans Gastroenterology.2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#AST#
25
#Gastroenterol#
29
#TRA#
23
#GAS#
34
#发病率#
33
#Gastroenterology#
25
#难治性#
21
谢谢!最新的信息读起来就是收获大
46