J Clin Oncol:Romyelocel-L可显著降低AML患者诱导化疗期间的感染风险
2021-06-24 MedSci原创 MedSci原创
Romyelocel-L或可成为降低接受诱导治疗的AML患者的感染风险的新选择
急性髓系白血病 (AML) 的标准细胞毒性诱导化疗可导致中性粒细胞减少症持续时间延长,感染风险增加。Romyelocel-L是一种通用的同种异体骨髓祖细胞制品,正在被研究用于减少诱导化疗期间的感染。
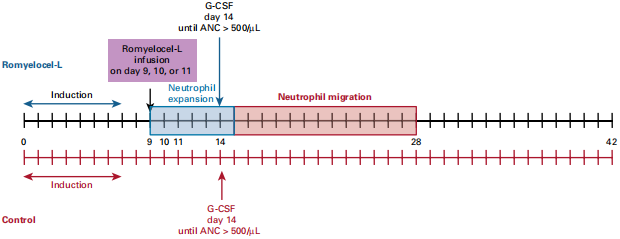
共163位接受诱导化疗的新发AML患者(≥55岁)在基线(第 0 天,d0)被随机分至治疗组和对照组,其中120位可评估。治疗组受试者在第 9 天接受输注Romyelocel-L,并从第14天起开始每天输注粒细胞集落刺激因子 (G-CSF) ,对照组仅从第14天起输注G-CSF,直到中性粒细胞绝对计数恢复到500/μL。
研究干预示意图
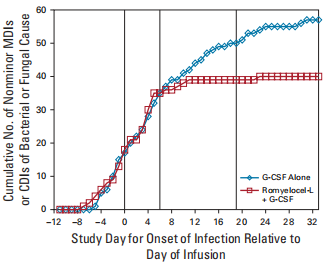
从第15-28天期间,治疗组的发热发作平均天数较对照组短(2.36 vs 3,.90, p=0.02)。与此类似,从第9-28天期间,治疗组中根据微生物学定义的感染和临床诊断的感染相比对照组表现出减少的趋势(35.6% vs 47.5%,p=0.002)。因此,治疗组中治疗感染的抗菌药或抗真菌药的使用量明显较对照组减少(第9-28天:44.1% vs 63.9%, p=0.01)。从第9-28天和第15-28天期间,治疗组接受经验性抗菌药物治疗的比例较对照组均明显降低(42.4% vs 63.9%,p=0.02;42.4% vs 62.3%,p=0.02)。
两组患者诱导化疗期间的汇总累积感染率
治疗组患者的住院时间也比对照组减少了3.2天(25.5 vs 28.7,p=0.001)。两组的缓解率和中性粒细胞计数绝对恢复的天数相似。治疗组无患者因感染而死亡,而对照组有两位患者死于感染。未观察到移植物抗宿主病。
综上所述,接受Romyelocel-L治疗的受试者的感染率、抗菌素使用率和住院率均有所降低,表明Romyelocel-L或可成为降低接受诱导治疗的AML患者的感染风险的新选择。
原始出处:
Desai Pinkal M,Brown Janice,Gill Saar et al. Open-Label Phase II Prospective, Randomized, Controlled Study of Romyelocel-L Myeloid Progenitor Cells to Reduce Infection During Induction Chemotherapy for Acute Myeloid Leukemia.[J] .J Clin Oncol, 2021, undefined: JCO2001739. https://doi.org/10.1200/JCO.20.01739
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Oncol#
34
#CEL#
0
#诱导化疗#
31
学习了,拥有
63
谢谢梅斯分享这么多精彩信息
53