Front Immunol:高中性粒细胞与淋巴细胞比值是终末期IgA肾病的独立危险因素
2022-01-26 从医路漫漫 MedSci原创
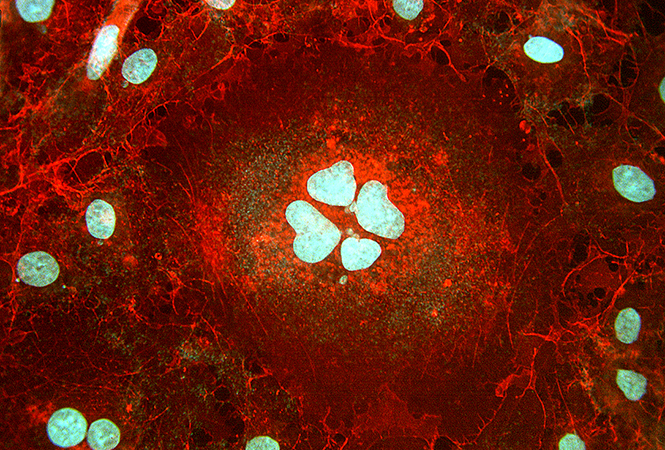
免疫球蛋白A肾病(IgAN)是世界范围内常见的原发性肾小球肾炎,其发生发展受多种因素的影响。
背景:免疫球蛋白A肾病(IgAN)是世界范围内常见的原发性肾小球肾炎,其发生发展受多种因素的影响。自身免疫和炎症被认为是其基本机制,但其确切发病机制尚不清楚。中性粒细胞/淋巴细胞比率(NLR)作为一种新的炎症标志物,已在多种疾病中得到研究。目前尚不清楚NLR能否预测IgAN患者的肾脏结局。我们评估了IgAN患者NLR与肾功能、病理损害、肾脏进展和预后的关系。
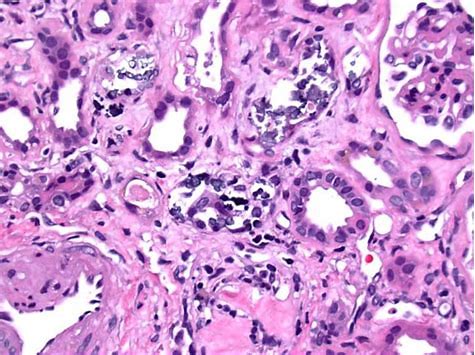
方法:对966例经活检证实的IgAN患者进行回顾性研究。根据NLR值分为高组(NLR2.6 7,n=384)和低组(≥<2.6 7,n=5 82)。终点为终末期肾病[估计肾小球滤过率(EGFR)<15mL/min/1.73m2或接受肾脏替代治疗]。对NLR与其他重要指标(EGFR、血肌酐、蛋白尿、高血压、肾脏病理损害)进行相关性检验。预测值由受试者工作特征曲线下面积(AUROC)决定。采用Kaplan-Meier和Cox比例风险分析评估肾脏进展和预后。
结果:NLR的AUROC最高,为0.633(P<0.001)。相关分析显示,NLR值与血肌酐(r=0.127,p<0.001)、24小时尿蛋白定量(r=0.18p<0.001)呈正相关,与表皮生长因子受体呈负相关(r=0.14p<0.001)。NLR值高的IgAN患者更易患高血压(p=0.003)。多因素Cox回归分析显示,即使在调整了重要的临床和病理参数后,高NLR值仍是IgAN的独立危险因素(p=0.043,HR=1.74,95%CI:1.0 2~2.97)。Kaplan-Meier分析显示,高NLR值与IgA肾病患者的肾脏预后显著相关(P<0.001),尤其是3~4期慢性肾病患者(P=0.028)或24小时尿蛋白定量>1g/d的患者(P<0.001)。
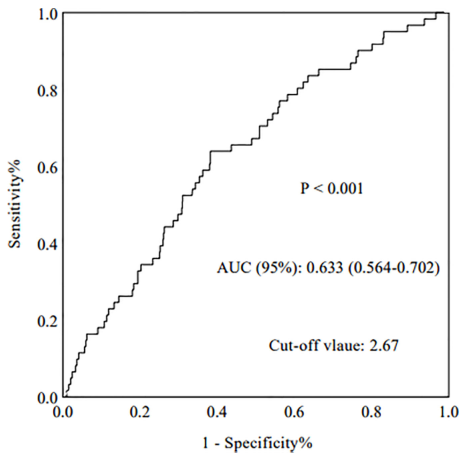
图1 NLR的ROC曲线下面积(AUC)。
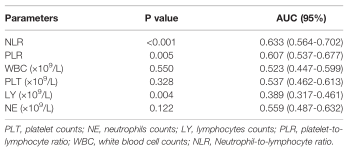
表1 各种预测因素对IgAN患者终末期肾病诊断的准确性

表2 966例IgAN患者的人口学和临床病理特征
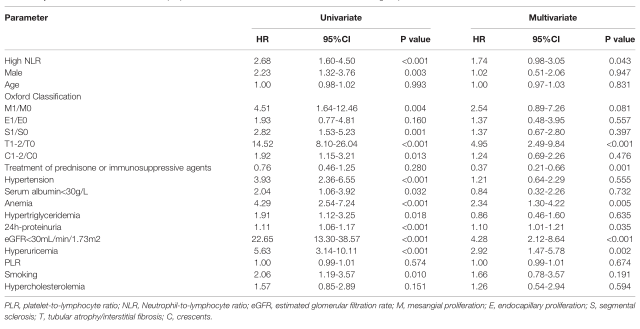
表3 966例IgAN患者肾脏预后的单因素和多因素Cox比例风险模型分析

图2 终末期肾病终点的不同类型Kaplan-Meier分析。(A)对所有患者进行Kaplan-Meier分析,直至终末期肾病(ESRD)终点。(B,C)对终末期肾病(ESRD)终点采用不同治疗方法的患者进行Kaplan Meier分析。(D-F)Kaplan-Meier分析对不同CKD分期到终末期的ESRD患者。(G,H)Kaplan-Meier分析不同尿蛋白患者的终末期肾病。
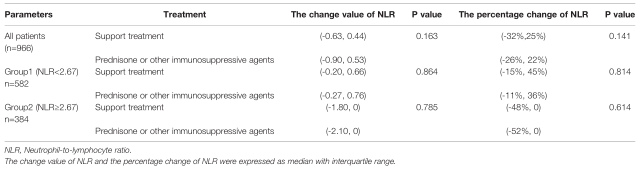
表4 966例患者治疗后NLR的变化
结论:NLR升高影响IgAN患者肾脏进展和预后,可作为评估肾功能和病理损害的指标。
原文出处:Wang S, Dong L, Pei G,et al.High Neutrophil-To-Lymphocyte Ratio Is an Independent Risk Factor for End Stage Renal Diseases in IgA Nephropathy.Front Immunol 2021;12
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#终末期#
41
#独立危险因素#
39
很有用
43
#中性粒细胞#
40
#淋巴细胞#
0
#IgA肾病#
41
#IgA#
21