CLIN CANCER RES:三阴性乳腺癌患者新辅助卡铂联合多西紫杉醇治疗后病情缓解情况及预后
2018-12-13 MedSci MedSci原创
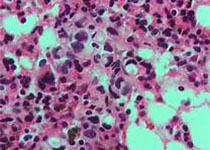
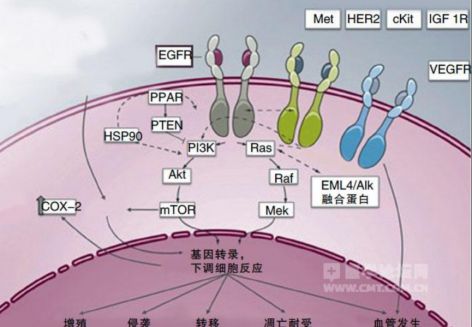
三阴性乳腺癌(TNBC)接受无蒽环霉素铂联合紫杉烷新辅助化疗(NAC)后达到病理完全缓解(pCR)情况以及病理缓解程度对预后的价值尚不清楚。CLIN CANCER RES近期发表了一篇文章,报告了卡铂联合多西紫杉醇NAC治疗后患者不同病理缓解程度的无复发生存(RFS)和总生存(OS)情况。
三阴性乳腺癌(TNBC)接受无蒽环霉素铂联合紫杉烷新辅助化疗(NAC)后达到病理完全缓解(pCR)情况以及病理缓解程度对预后的价值尚不清楚。CLIN CANCER RES近期发表了一篇文章,报告了卡铂联合多西紫杉醇NAC治疗后患者不同病理缓解程度的无复发生存(RFS)和总生存(OS)情况。
190名患有I-III期TNBC的患者接受6个周期,每周期21天的新辅助卡铂(AUC6)联合多西紫杉醇(75mg / m 2)治疗。对治疗后pCR(乳房和腋窝无侵袭性肿瘤)和残余肿瘤负担(RCB)进行评估。随访患者的复发和存活情况。使用Kaplan-Meier方法分析病理反应的程度与RFS和OS的相关性。患者中位年龄为51岁,52%为淋巴结阳性。pCR和RCB I率分别为55%和13%。5%的pCR患者,0%的RCB I患者和58%的RCB II / III患者接受了辅助性蒽环类治疗。三年RFS和OS分别为79%和87%。达到pCR患者的三年RFS为90%,未到达pCR的患者为66%。达到pCR患者的三年OS为94%,未到达pCR的患者为79%。RCB I患者3年RFS(93%)和OS(100%)与达到pCR的患者相似。多因素分析表明,肿瘤分期较晚,淋巴结阳性和RCB II / III与较差的RFS相关。
文章最后认为,新辅助卡铂联合多西紫杉醇在TNBC中具有良好的疗效。使用该治疗方案达到pCR或RCB I的患者3年RFS和OS良好。
原始出处:
Priyanka Sharma, Sara López-Tarruella, et al. Pathological Response and Survival in Triple-Negative Breast Cancer Following Neoadjuvant Carboplatin plus Docetaxel. CLIN CANCER RES. December 2018 doi: 10.1158/1078-0432.CCR-18-0585
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新辅助#
27
#铂#
24
#病情#
28
#阴性乳腺癌#
0
#卡铂#
29
#三阴性#
21
#乳腺癌患者#
26
#多西紫杉醇#
30