Lancet Respirat:预防性持续气道正压通气是否可减少腹部大手术的术后并发症?
2021-06-23 Nebula MedSci原创
CPAP并未降低腹部大手术后肺炎、气管内再插管或死亡的发生率
呼吸系统并发症是术后并发症的重要原因。本研究旨在调查腹部大手术后立即给予持续气道正压通气 (CPAP) 是否可以预防术后并发症。
PRISM是一项在6个国家的70家医院开展的开放标签的、随机的3期试验,招募了50岁及以上的择期进行开腹大手术的患者,1:1随机分至两组,在术后4小时内接受CPAP或常规术后护理。主要终点是分组后30天内肺炎、气管再插管或死亡的综合结局。
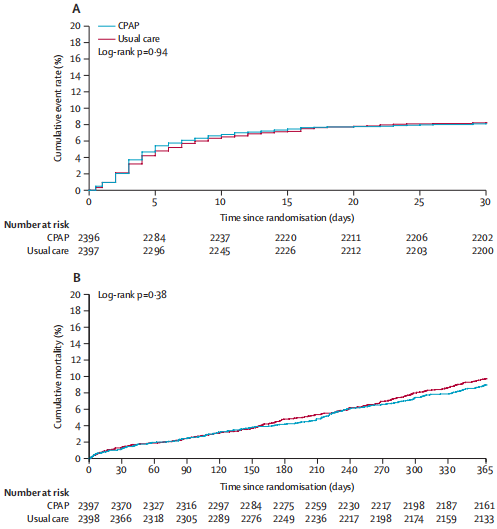
随机分组后30天和365天内的两组累积死亡率
2016年2月8日至2019年11月11日,共有4806位患者被随机分至CPAP组(n=2045)或常规护理组(n=2396),其中4793位被纳入了主要分析(CPAP组 2396人,常规护理组 2397人)。CPAP组2396位患者中有195位(8.1%)和常规护理组2397位患者中的197位(8.2%)患者达到了复合主要终点(校正优势比 1.01,p=0.95)。
CPAP组2241位患者中有200位(8.9%)患者发生了不良反应事件。最常见的不良反应事件有幽闭恐惧症(3.5%)、口鼻干燥(1.9%)、过度呼气(1.6%)、呕吐(1.2%)和疼痛(1.1%)。有两例重度不良反应:一位患者为明显的耳聋,一位患者因CPAP罩导致静脉导管阻塞,导致一过性的血流动力学不稳定。
综上,在这项大型临床有效性试验中,CPAP并未降低腹部大手术后肺炎、气管内再插管或死亡的发生率。因此,尽管CPAP在手术后呼吸衰竭的治疗中具有重要作用,但不推荐术后常规使用预防性CPAP。
原始出处:
Rupert Pearse, et al. Postoperative continuous positive airway pressure to prevent pneumonia, re-intubation, and death after major abdominal surgery (PRISM): a multicentre, open-label, randomised, phase 3 trial. The Lancet Respiratory Medicine. June 18, 2021. https://doi.org/10.1016/S2213-2600(21)00089-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#大手术#
42
#并发#
26
#正压通气#
37
#持续气道正压通气#
37
#Lancet#
36
#预防性#
27
顶刊就是不一样,质量很高,内容精彩!学到很多
49