Cell Reports:在严重癫痫发作后,小胶质细胞不仅清除碎片,而且还愈合受损的树突
2021-07-24 MedSci原创 MedSci原创
常见的预防癫痫药物对大约三分之一的癫痫患者无效,因此非常需要针对此类脑损伤的新的更好的治疗方法。癫痫发作是癫痫最明显的表现。在小鼠癫痫发作的临床前模型中,长时间的癫痫发作会导致树突损伤。并严重损害神经
常见的预防癫痫药物对大约三分之一的癫痫患者无效,因此非常需要针对此类脑损伤的新治疗方法。癫痫发作是癫痫最明显的表现,在小鼠癫痫发作的临床前模型中,长时间的癫痫发作会导致树突损伤,并严重损害神经元恢复。因此,有助于解决癫痫引起的树突状结构损伤的过程在治疗癫痫上是有益的。
小胶质细胞是主要的大脑驻留免疫细胞,有助于神经元结构和功能网络的发育和稳定性。小胶质细胞可用于改善癫痫发作的想法得到了越来越多的普遍支持,但一直缺乏直接的、可视化的证据来证明它们如何做到这一点。
为解决这一问题,研究员在红藻氨酸 (KA) 诱导的癫痫发作后对转基因小鼠中的小胶质细胞和神经元进行了双光子成像,研究结果发现,在严重癫痫发作后,严重的癫痫发作会诱导小胶质细胞过程袋的形成,小胶质细胞通过与神经元树突的物理相互作用从而愈合受损的树突。该研究结果发表在 Cell Reports上。

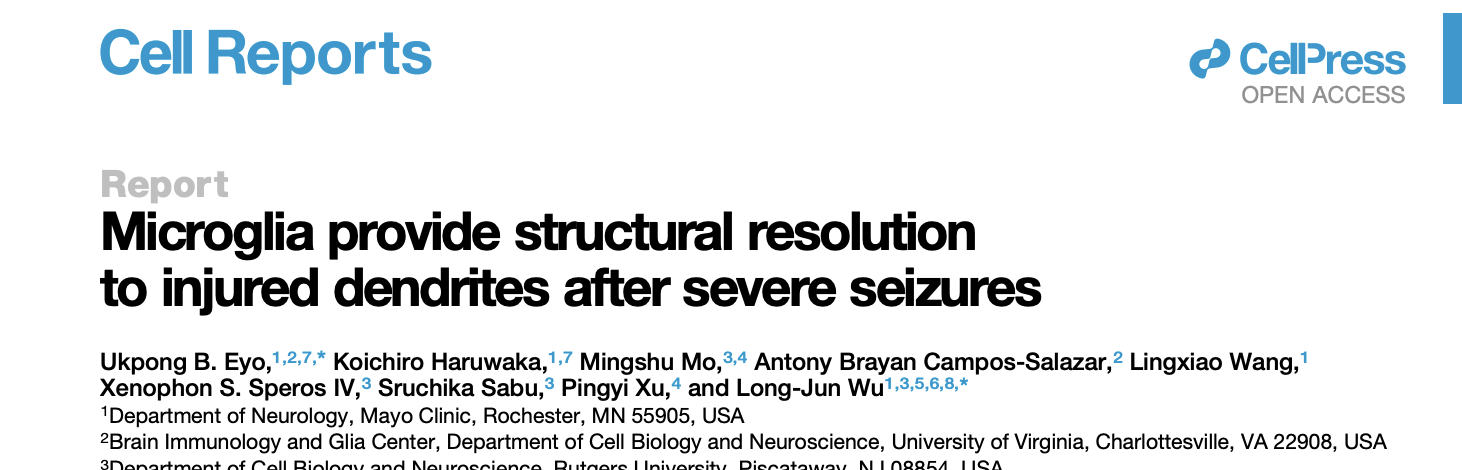
在该研究中,研究员使用双光子显微镜的先进成像技术来检查实验室小鼠在严重癫痫发作后大脑中发生的情况。他们第一次观察到,小胶质细胞不是简单地清理碎片,而是开始形成小袋。这些小袋并没有像许多免疫细胞那样吞噬受损物质。相反,它们开始照顾肿胀的树突--传递神经冲动的神经细胞分支。科学家们意识到,它们不是在清除,它们似乎正在愈合树突。
癫痫发作引起的小胶质细胞过程袋的实时动态变化
这些奇怪的小袋子——科学家们将它们命名为“小胶质过程袋子”——在那里呆了几个小时。他们经常缩小,但他们显然在做一些有益的事情,因为他们瞄准的树突最终看起来比他们没有瞄准的树突更好、更健康。
综上所述,研究员记录了一种小胶质细胞表型,并称之为小胶质细胞过程袋或 MPP,它在严重癫痫发作后被强烈诱导,缠绕在珠状树突周围,并稳定维持数小时,保存它们的趋化能力。
参考文献:Ukpong B. Eyo et al, Microglia provide structural resolution to injured dendrites after severe seizures, Cell Reports (2021). DOI: 10.1016/j.celrep.2021.109080
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#Cell#
45
#CEL#
41
#胶质细胞#
36
理学物理试验
68
梅斯理学计较
59