JAHA:与院内心脏骤停相关特征和结局的时间趋势
2021-12-04 MedSci原创 MedSci原创
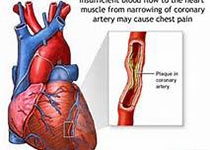
在美国,院内心脏骤停(IHCA)的年发生率估计约为300000例。根据英国和美国的数据,每1000例住院患者分被有1.6至2.85例。可电击复律(无脉冲室性心动过速/心室颤动[VT/VF])占这些心律
在美国,院内心脏骤停(IHCA)的年发生率估计约为300000例。根据英国和美国的数据,每1000例住院患者分被有1.6至2.85例。可电击复律(无脉冲室性心动过速/心室颤动[VT/VF])占这些心律失常事件的15.3%,其余为无脉冲电活动(PEA)-心搏停止。尽管复苏医学取得了进步,但IHCA的医疗负担仍然很大。这些进步和复苏指南的变化对IHCA生存率的影响仍未明确。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,为了更好地描述IHCA性质和结局不断变化的患者特征和趋势,研究人员对国家数据库进行了20年的随访分析。研究人员使用国际疾病分类、第九次修订和第十次修订的临床代码(ICD-9-CM和ICD-10-CM)分析了全国住院患者样本(1999-2018),以确定所有IHCA的成年患者。研究人员根据心脏骤停的类型(即室性心动过速/心室颤动或无脉搏电活动-心搏停止)进行亚组分析。年龄和性别调整模型和多变量风险调整模型用于调整潜在的混杂因素。

在20年的研究期间,研究人员观察到IHCA的发生率稳步上升,主要亚组为无脉冲电活动-心搏停止。总体而言,在调整风险因素后,存活率提高了10%以上。近年来(2014-2018),研究人员注意到生存率提高的类似趋势,尽管这仅在无脉搏电活动-心搏停止队列中取得了统计学意义。

尽管IHCA复苏理想的质量指标是有意义的神经功能恢复,但患者生存下来是实现这一目标的第一步。随着整体IHCA发生率的上升,整体存活率也在同步提高。然而,近年来,这些改善趋于平稳,尤其是在室性心动过速/心室颤动相关存活率方面。未来的工作需要更好地识别IHCA非幸存者的特征,以改善该领域的资源分配和医疗保健政策。
原始出处:
Lingling Wu,et al.Temporal Trends in Characteristics and Outcomes Associated With In‐Hospital Cardiac Arrest: A 20‐Year Analysis (1999–2018).JAHA.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.021572
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#时间趋势#
0
#院内心脏骤停#
38
👍👍👍👍👍
55
#AHA#
29
新的方向
49
可以的
46
学习了
50