J Thorac Oncol: RNA深度测序显示融合异质性可预测克唑替尼对ALK重排非小细胞肺癌的治疗效果
2021-10-11 yd2015 MedSci原创
研究表明,肿瘤内EML4-ALK亚型可预测ALK重排非小细胞肺癌(NSCLC)患者靶向治疗的疗效。
ALK重排非小细胞肺癌(NSCLC)的基因融合变异有可能预测患者的预后,但以前的研究结果还不确定。同一肿瘤中融合异构体共存可能影响靶向治疗的疗效,但尚未进行相关研究。因此,来自我国香港、浙江、江苏等地的学者开展了相关研究,评估其对于克唑替尼疗效预测价值。成果发表在J Thorac Oncol杂志上。
研究纳入51名符合纳入标准的非小细胞肺癌患者,随访至2020年12月31日。包括33名女性(65.0%)和18名男性(35.0%),诊断时的平均年龄为53.8岁(范围29-76岁)。37.3%的患者ECOG评分为0分,其余患者为1分。吸烟患者占21.6%,脑转移患者占33.3%。
使用单管RNA和DNA测序方法,检测EML4-ALK变异类型。两个主要变异类型是v1 (n = 23;45.1%)和v3 (n = 19;37.3%),其次为v2 (n = 5;9.8%), v5, (n = 3;5.9%)和v5 (n = 1;2.0%)。24例(47.1%)肿瘤中检测到多种EML4-ALK亚型,27例(52.9%)肿瘤中检测到单一亚型。大多数v3肿瘤(16/19, 84.2%)同时存在v3a和v3b转录亚型。多亚型在v3肿瘤中比在非v3肿瘤更常见(P<0.001)。
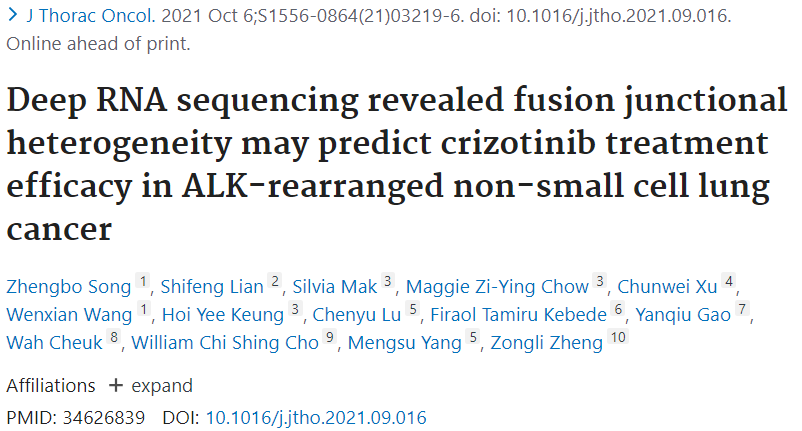
v3肿瘤患者与非v3肿瘤患者的PFS差异无统计学意义(中位PFS: 8.9 m vs 13.8 m, P = 0.082)。存在多亚型患者的PFS明显短于单亚型患者(中位PFS: 8.9 m vs 15.9 m, P = 0.006)。存在多亚型患者中,v3肿瘤患者和非v3肿瘤患者的PFS仍然无差异(中位PFS: 9.0 m vs 7.6 m;P = 0.928)。相反,在非v3患者中,存在多亚型患者的PFS同样短于单亚型患者(中位PFS: 7.6 m vs 15.9 m;P = 0.045)。
PFS
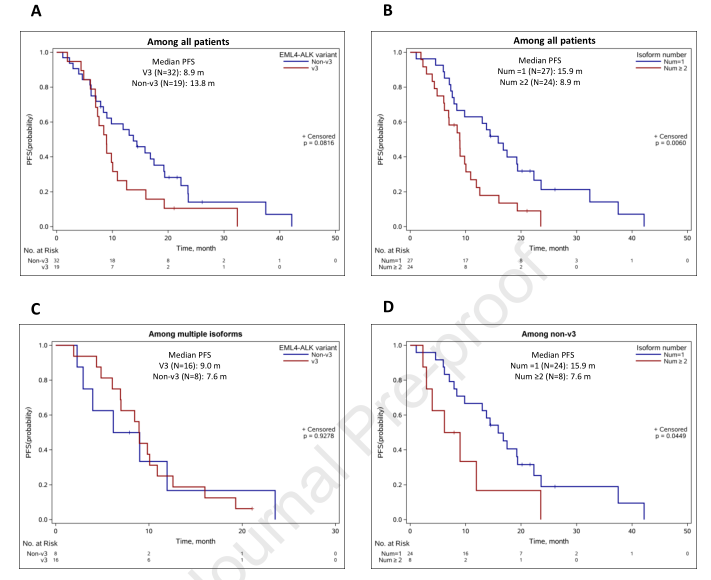
Cox回归分析显示,v3和非v3肿瘤患者对比,PFS在单因素模型(HR [95% CI]: 1.72[0.93 - 3.18])和多因素模型(HR [95% CI]: 1.05 [0.45 2.43])均没有统计学差异。与单亚型患者相比,多亚型组的PFS较差,在单变量模型中差异有统计学意义(HR [95% CI]: 2.37 [1.26 - 4.45]),同样在调整潜在混杂因素后的多变量模型(HR [95% CI]: 2.45 [1.06 5.69])中差异也有统计学差异。在分层分析中,在多亚型患者中,v3变异类型与PFS无关(HR [95% CI]:单变量0.96[0.37 - 2.48],多变量1.03 [0.35 - 3.08])。与Kaplan-Meier分析一致,在非v3肿瘤患者中,与单亚型相比,多亚型与更差的PFS相关(HR [95% CI]:单变量2.44[0.99 - 6.02]和多变量3.68 [1.21 - 11.21])。
PFS和OS相关因素分析
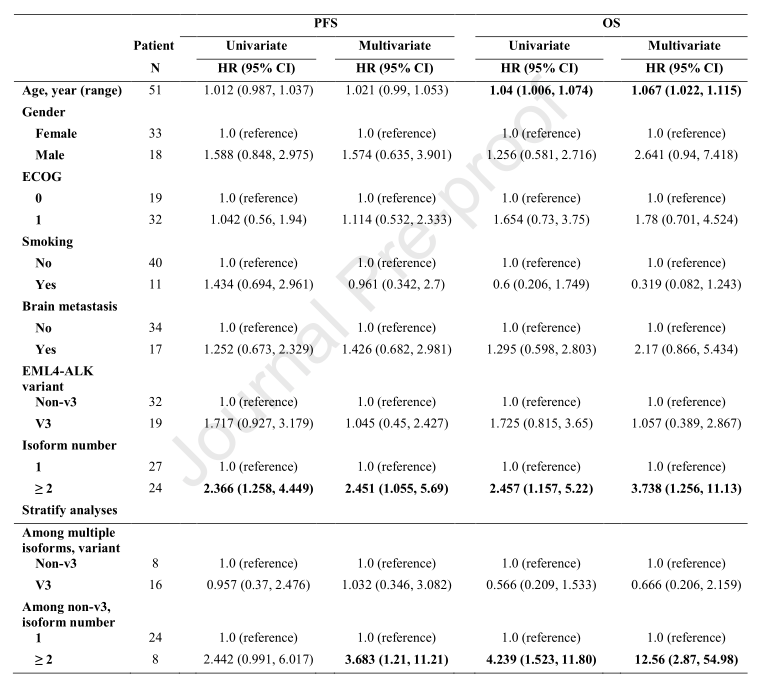
v3患者的生存期(OS)短于非v3患者,但差异无统计学意义(中位生存期:21.6 m vs 38.5 m, P = 0.149)。多亚型患者的OS比单亚型肿瘤患者的OS短(中位OS: 18.5 m vs 49.8 m;P = 0.016)。在分层分析中,在多亚型患者中,融合变异类型与OS无关(中位OS: v3 vs非v3: 21.6 m vs 16.5 m;P = 0.257)。然而,在非v3患者中,多亚型与更短的OS相关(中位OS: 16.5 m vs 49.8 m;P = 0.003)。
OS
在单变量Cox回归中,与OS相关的唯一基线临床特征是年龄(HR [95% CI]: 1.04 [1.01 - 1.07]; v3肿瘤患者的OS与非v3患者相比在校正前(HR [95% CI]: 1.73[0.82 - 3.65])和校正潜在混杂因素后(HR [95% CI]: 1.06[0.39 - 2.87])均无统计学差异。同时,在调整潜在混杂因素之前和之后,与单亚型相比,多亚型患者与较高的死亡风险相关(HR [95% CI]: 2.46[1.16 - 5.22]和3.74[1.26 11.13])。在分层分析中,融合变异类型与OS无关(HR [95% CI]:单变量0.57[0.21 - 1.53],多变量0.67[0.21-2.16])。在非v3组中,与单亚型相比,多亚型与较高的死亡风险相关(校正潜在混杂因素后,单变量模型的HR=4.24,[95% CI] [1.52 - 11.80]) ,和多变量模型的HR=12.56,[95% CI]: [2.87 - 54.98])。
综上,研究表明,肿瘤内EML4-ALK亚型可预测ALK重排非小细胞肺癌(NSCLC)患者靶向治疗的疗效。
原始出处:
Song Z, Lian S, Mak S, Chow MZ, Xu C, Wang W, Keung HY, Lu C, Kebede FT, Gao Y, Cheuk W, Cho WCS, Yang M, Zheng Z. Deep RNA sequencing revealed fusion junctional heterogeneity may predict crizotinib treatment efficacy in ALK-rearranged non-small cell lung cancer. J Thorac Oncol. 2021 Oct 6:S1556-0864(21)03219-6. doi: 10.1016/j.jtho.2021.09.016. Epub ahead of print. PMID: 34626839.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#治疗效果#
36
#深度测序#
39
#THORAC#
31
#Oncol#
0
#非小细胞#
31
#融合#
44