JACC:ST段抬高型心肌梗死患者急性心衰的发生和预后存在性别差异
2019-11-06 不详 MedSci原创
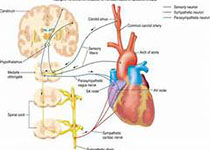
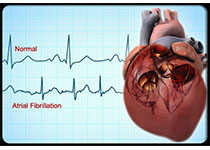
ST段抬高型心肌梗死(STEMI)合并急性心衰症状与死亡率增高有关。然而心衰的发展和预后是否存在性别差异尚不清楚。本研究的目的旨在评估STEMI患者性别、急性心衰和预后的相关性。本研究纳入分析了ISACS-TC数据库中的患者,主要终点事件是住院期间心衰Killip分级≥II和30天死亡风险。最终共纳入了10443名患者(女性占3112名),经多变量分析调整后发现,女性患者的新发急性心衰发生率明显高
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JACC#
31
#ACC#
0
#急性心衰#
50
#ST段抬高#
42
#ST段#
38
学习
86