欧洲心脏杂志研究称:未放支架的心梗患者,或应长期双抗治疗
2019-12-15 朱朱 中国循环杂志
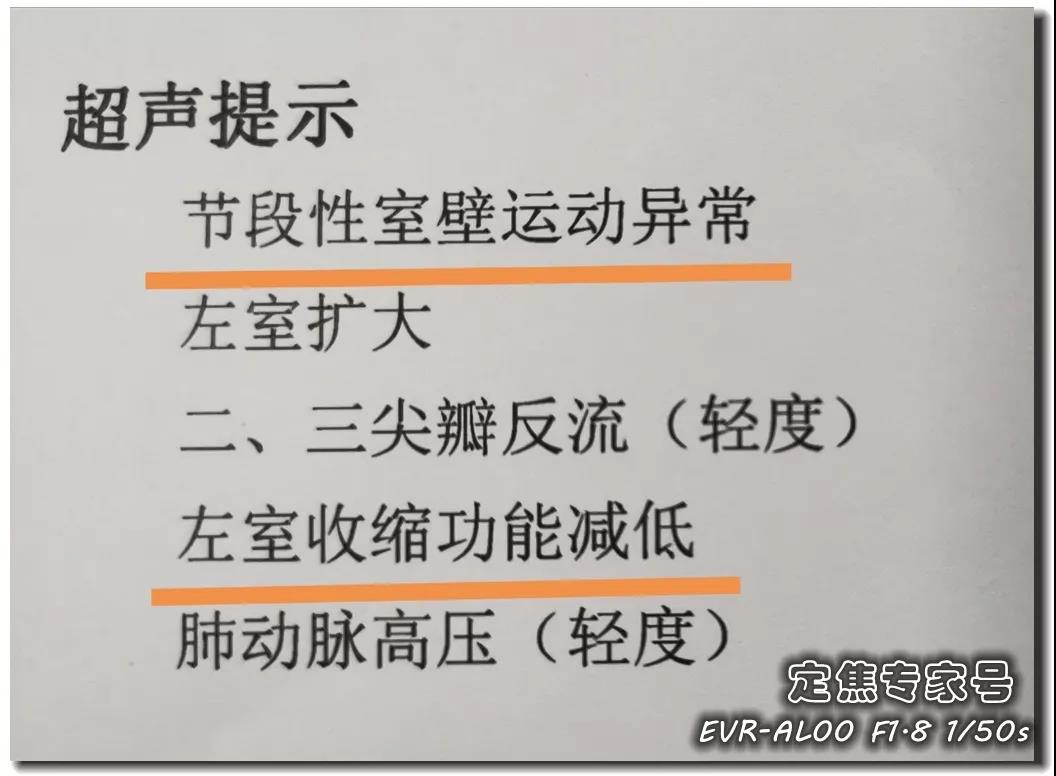
对于冠脉支架术后的稳定性冠心病患者,近年来不少研究表明,短时程的双联抗血小板治疗时程在疗效上不劣于长时程的治疗,而且更加安全。此前公布的PEGASUS-TIMI 54研究结果提示,在既往发生过心梗的患者中,应用阿司匹林和替格瑞洛进行长期(1年以上)双联抗血小板治疗可显着降低主要不良心血管事件风险,出血发生率轻微升高,但在可接受范围内。但之前主要聚焦于放冠脉支架的患者。近日,《欧洲心脏杂志》发表的P
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#心梗患者#
46
#欧洲#
28
#双抗治疗#
37
#双抗#
35
学习了
82
好好好好好好
51
学习了,谢谢分享
66