胸双侧交感神经切除术作为肺动脉高压治疗的新方法:证据不足
2022-01-14 刘少飞 MedSci原创
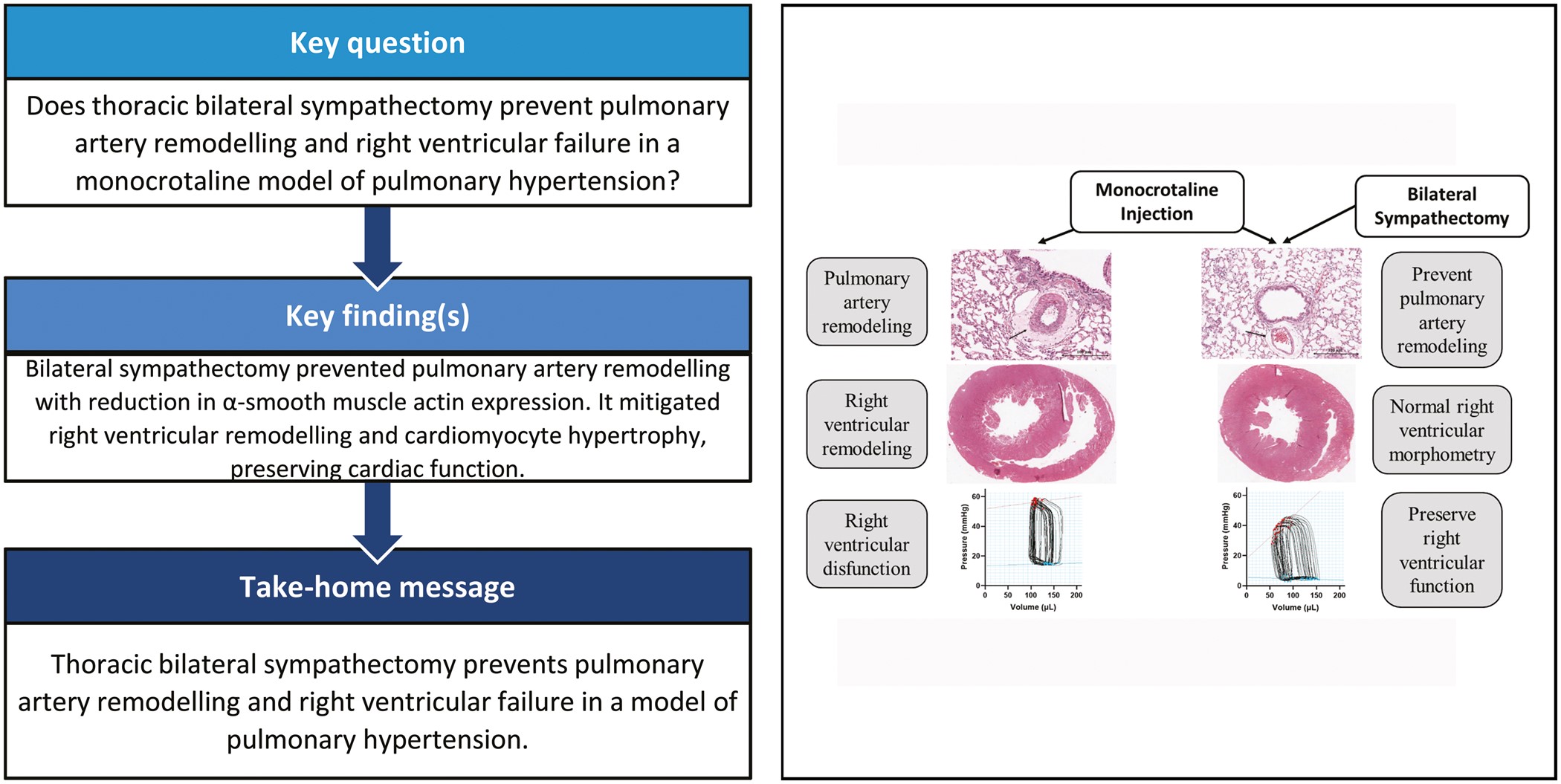
肺动脉高压 (PH) 是一种临床综合征,其特征是肺循环压力慢性进行性增加,导致右心衰竭并最终死亡。双侧交感神经切除术对大鼠实验性肺动脉高压 (PAH) 动力学的影响是相关的。
肺动脉高压 (PH) 是一种临床综合征,其特征是肺循环压力慢性进行性增加,导致右心衰竭并最终死亡。治疗选择在方法和应用时间方面都是有限的,并且通常是姑息性的。在这种情况下,描述双侧交感神经切除术对大鼠实验性肺动脉高压 (PAH) 动力学的影响是相关的。应该强调的是,交感神经切除术尚未包括在临床实践中用于 PAH 治疗的工具库中;最常见的手术方法是房间隔造口术或 Potts 分流术。一个全新的方向是血管内肺动脉去神经术(冷冻或射频),但是目前对肺动脉去神经术作为治疗方法证据依然不足。
证据1. 肺动脉高压的一般概念
肺循环的结构特征包括容易伸展的毛细血管网络,它对右心室的工作阻力很小,它很容易应对容量,但不能很好地适应压力过载。在休息时,只有大约 1/10 的肺组织在起作用,而在其余不通气的区域,血流通过动静脉吻合口分流,不仅绕过毛细血管,还绕过小动脉。对于PAH,这很重要,因为这意味着存在补偿机制,可以在很长一段时间内避免与小动脉管腔减少相关的负面后果。例如,从血流中排除甚至一半的肺血管体积(例如作为全肺切除术的结果)几乎不会导致 PH 的发展。因此,肺小动脉因壁受损而关闭并不总是 PH 的唯一和决定性原因。
证据2. 肺动脉高压的形式
我们应该清楚地了解,该研究的主要进行的实验仅模拟(而不是在所有方面)最常见的一种 PH 形式—特发性PAH(根据现代分类的第1组)。然而,除了原发性之外,PH 可能是继发性病理过程,是由于先前的心脏、肺和其他疾病而发展起来的。同时,左右分流的二尖瓣狭窄、肺栓塞或先天性心脏缺陷的PH发病机制不同。在所有这些情况下,任何试图影响 PH 而不消除主要原因的尝试都是没有意义的。因此,交感神经切除术可能有用,至少在理论上,仅对毛细血管前PH值有用;除此之外,它仅在血管收缩未转化为肺血管玻璃样变之前的阶段才有可能产生影响。
证据3. 实验概念和结果
在3周内诱导 PAH 的实验性野百合碱模型不太可能对应于人类多年来发生的那些长期补偿和病理过程。然而,实验概念中最不设防的环节应该是,它的设计仅假设“预防性”交感神经切除术(在 PAH 建模开始之前)。这种“相反”的事件序列并未提供交感神经切除术在 PAH 中潜在有益作用的证据。对手稿中提供的数据的分析可以得出结论,就许多研究的血流动力学参数而言,结果不仅在组之间而且在组内部也存在显着差异(高达 50 倍)。这种分散可能表明,即使在最标准化的实验条件下,也没有发生结果的完全可复制性,即适应性和病理机制分别以不同的方式进行。造成这种差异的原因我们仍然不完全清楚。
证据4. 从动物模型到人体的转化困难
主要问题仍然存在:是否有可能将这种手术干预转化为真正的临床实践?显然,这个问题存在(并将存在):“……没有一种动物模型可以准确地复制人类疾病,甚至只关注其中一个 PH 组”。应考虑实验动物和人类之间的解剖学和生理学差异。关于研究主题:在啮齿动物中,传出(交感神经和副交感神经)血管周围轴突终止于大血管,而在人类中,这种神经支配延伸到肺内小血管。同时,正如在一项研究中显示的那样,血管对血管活性剂的反应也随着动脉口径的减小而降低。特别是,其中一个结论如下:“……去甲肾上腺素是诱导肺外动脉收缩的神经递质。去甲肾上腺素和交感神经在肺内动脉中的作用似乎不太重要。
尤其是与在 PAH 治疗中使用 β 受体阻滞剂相关的讨论,这在实验中显示出令人鼓舞的结果,但并未伴随对患者的积极影响。因此,在其他的研究中指出:“β-肾上腺素受体阻滞剂……在肺动脉高压的情况下具有潜在危险。在这种情况下,它们的负性肌力和变时作用难以耐受,心脏储备因每搏输出量的减少和固定而受损,并且它们的给药可导致显着的心肺功能损害。这不是一个新发现,但在日常临床实践中却鲜为人知”。总之,尽管存在一些局限性,但这项由国际研究团队在非常高的方法学水平上进行的有趣研究,可以扩展知识并更好地了解 PAH 发展过程中肺血管和心肌的病理过程。毫无疑问,这方面的研究应该继续下去。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#新方法#
44
#切除术#
43
#动脉高压#
37
#高压治疗#
0
肺动脉高压治疗难度大,仍是难点
56
学习#学习#
50
#双侧#
0