在需求激增的情况下,葛兰素史克和Vir提高了COVID-19抗体疗法Sotrovimab的产量
2022-01-23 Allan MedSci原创
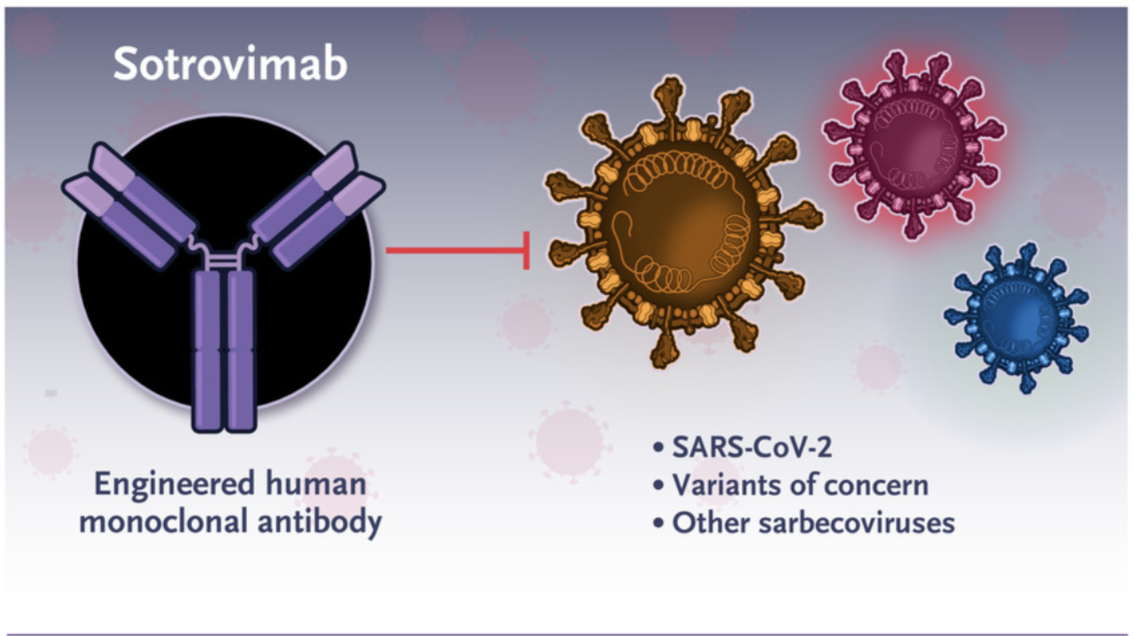
葛兰素史克和 Vir 发布了来自临床前研究的数据,结果显示sotrovimab保留了针对 Omicron 刺突蛋白的体外活性,尽管该毒株存在许多突变。
葛兰素史克和其合作伙伴 Vir Biotechnology 正在第二家工厂提高其COVID-19抗体治疗药物 sotrovimab 的产量,以跟上激增的需求。Omicron 变体的迅速出现进一步加剧了供应压力,这使得 Regeneron Pharmaceuticals 和 Eli Lilly 的竞争性抗体基本上无效。
Sotrovimab 已在包括美国在内的多个国家获得批准,用于高风险的轻度至中度 COVID-19 患者。自 11 月下旬 Omicron 出现以来,葛兰素史克和 Vir 发布了来自临床前研究的数据,结果显示sotrovimab保留了针对 Omicron 刺突蛋白的体外活性,尽管该毒株存在许多突变。

由药明康德在上海经营的一家工厂一直负责 sotrovimab 的制造,但自从 Omicron 出现以来,葛兰素史克和 Vir 通过增加另一家由三星生物制品公司经营的工厂来加速提高产量。然而,虽然三星工厂已经在增加全球供应,但它可能需要几个月的时间才能满负荷运转。同时,葛兰素史克还调整了意大利帕尔马工厂的供应线。
供应的另一个压力是,已发现 Omicron 可以逃避许多其他针对 COVID-19 的单克隆抗体,包括 Regeneron 的 REGEN-COV,以及礼来(Eli Lilly)的 bamlanivimab 与 etesevimab 联合疗法。在最近更新的 COVID-19 治疗指南中,鉴于 Omicron 在全世界的主导地位,美国国立卫生研究院 (NIH) 现在建议不要使用 Regeneron 和礼来(Eli Lilly)的抗体疗法。
尽管有新的建议,但美国一些单克隆抗体供应稀缺的州继续使用这两种新近无效的治疗方法。最近对联邦数据的分析发现,在佛罗里达州、加利福尼亚州和纽约州等十几个州,Regeneron 和礼来公司抗体疗法的使用率最高。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#mAb#
34
#激增#
33
#葛兰素史克#
30
#抗体疗法#
30
#OTR#
37
学习了
51
学习了,谢谢分享
55