间歇性禁食增强临床前肺动脉高压右心室功能
2021-11-10 刘少飞 MedSci原创
间歇性禁食 (IF) 具有多效性心血管益处,包括肠道微生物组的重组和细胞代谢的增强。间歇性禁食将如何改变肺动脉高压的野百合碱模型中的肠道微生物群组成、右心室功能和存活率。
间歇性禁食 (IF) 是一种新兴的多种慢性疾病的非药物干预措施,因为它能够延长从单细胞生物到非人类灵长类动物的各种物种的寿命。 IF 的好处是多方面的,但提出的机制包括增强细胞代谢和肠道微生物组的重组。微生物群产生代谢物,如短链脂肪酸、氨基酸和胆汁酸,可调节宿主代谢、免疫反应和肠道稳态。微生物群代谢物的调节对于正常生理机能至关重要,因为微生物群失调与多种疾病有关。
肺动脉高压 (PAH) 是一种罕见但致命的疾病,其特征是代谢缺陷和微生物群失调。右心室 (RV) 衰竭是 PAH 死亡的主要原因。 RV 代谢中断,包括线粒体脂肪酸氧化受损,导致脂毒性和神经酰胺积累。 RV 脂毒性被认为是导致 RV 功能障碍的重要因素,因为它存在于临床前和临床 PAH 中。
由于 IF 可纠正代谢缺陷并对抗肠道菌群失调,因此它可能是一种增强 PAH 中 RV 功能的非药物方法。为了研究这一假设,我们分析了 IF 对 PAH 的野百合碱大鼠模型中肠道微生物群组成、体重增加、RV 中微生物群代谢物丰度、RV 脂毒性、RV 功能和存活率的影响。
研究方法:
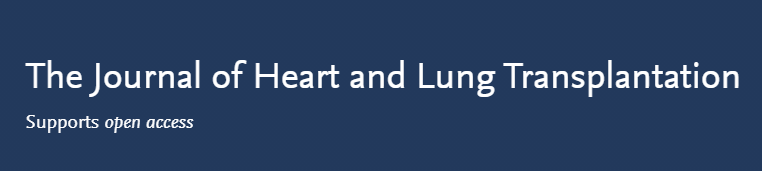
雄性 Sprague Dawley 大鼠随机分为 3 组:对照组、野百合碱随意喂养和野百合碱 IF(隔日喂养)。超声心动图和有创血流动力学显示 IF 改善了 RV 收缩和舒张功能,尽管 PAH 的严重程度没有显着变化。
研究结果:
IF 可防止过早死亡(野百合碱随意使用的死亡率为 30%,而野百合碱 IF 大鼠的死亡率为 0%,P=0.04)。 IF 降低了 RV 心肌细胞肥大并减少了 RV 纤维化。

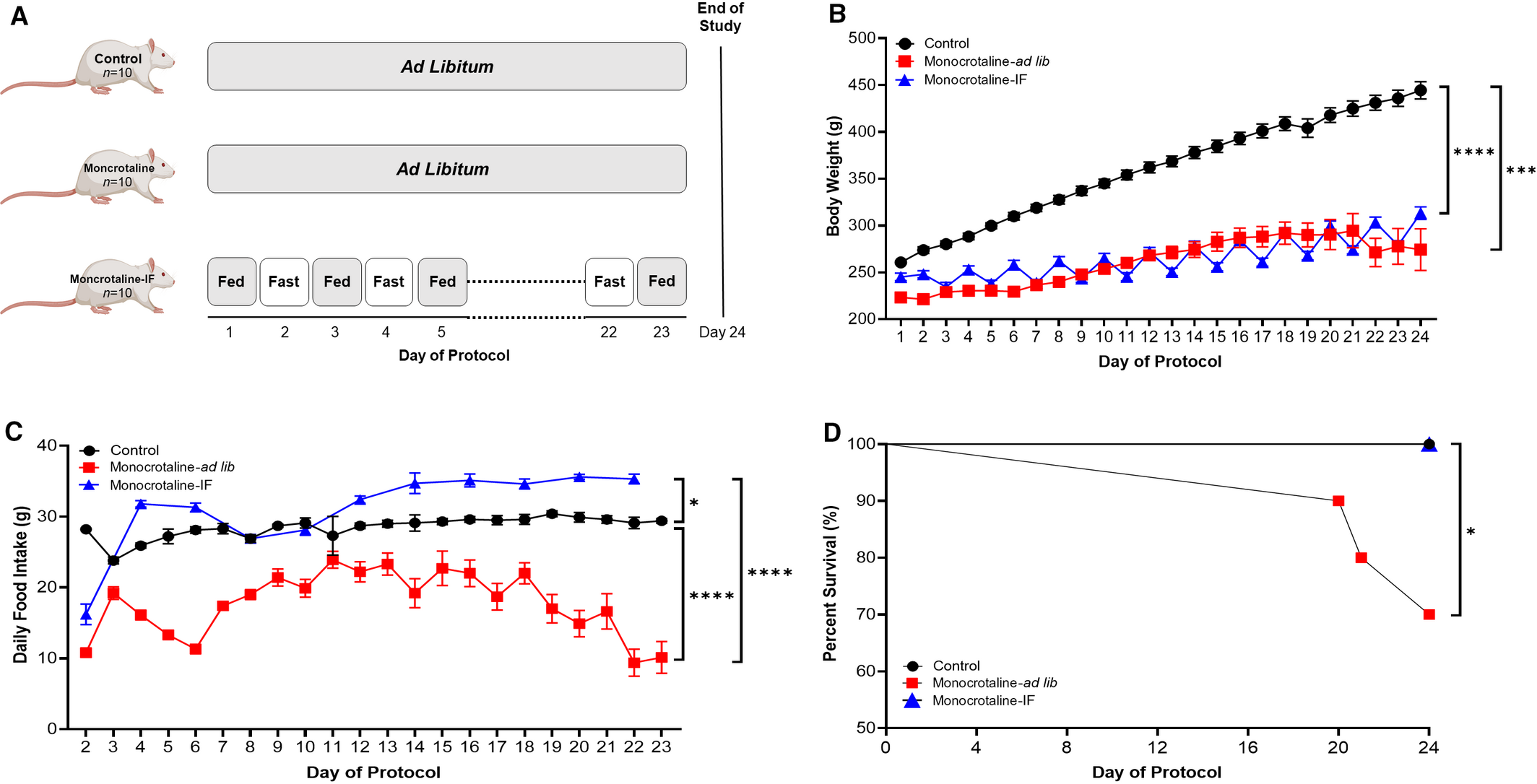
IF 阻止了油红 O 染色的 RV 脂质积累和代谢组学确定的神经酰胺积累。与野百合碱随意相比,IF 减轻了空肠绒毛长度和杯状细胞丰度的减少。 16S 核糖体 RNA 基因测序证明 IF 改变了肠道微生物组。
特别是,野百合碱-IF 大鼠中乳酸杆菌的丰度增加。代谢组学分析显示,IF 降低了微生物组代谢物的 RV 水平,包括胆汁酸、芳香族氨基酸代谢物和 γ-谷氨酸化氨基酸。
文章出处:
Prisco SZ, Eklund M, Moutsoglou DM, Prisco AR, Khoruts A, Weir EK, Thenappan T, Prins KW. Intermittent Fasting Enhances Right Ventricular Function in Preclinical Pulmonary Arterial Hypertension. J Am Heart Assoc. 2021 Nov 8:e022722. doi: 10.1161/JAHA.121.022722. Epub ahead of print. PMID: 34747187.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#右心室功能#
41
#动脉高压#
32
#间歇性#
46
#右心室#
37