JAMA:两个简单量表指导PFO闭合术的决策
2022-01-08 杨中华 “脑血管病及重症文献导读”公众号
在18-60岁青壮年和中年人缺血性卒中中,卵圆孔未闭(PFO)相关性卒中占10%。预防PFO相关缺血性卒中患者复发性卒中的治疗策略包括抗血栓治疗或经皮PFO封堵,每种治疗策略都在实践指南中得到认可。
在18-60岁青壮年和中年人缺血性卒中中,卵圆孔未闭(PFO)相关性卒中占10%。预防PFO相关缺血性卒中患者复发性卒中的治疗策略包括抗血栓治疗或经皮PFO封堵,每种治疗策略都在实践指南中得到认可。
已经完成了六项比较器械闭塞联合药物治疗与单独药物治疗的随机临床试验。研究水平的荟萃分析表明,闭塞与较低的缺血性卒中复发率相关。然而,对于一些接受药物治疗的患者来说,卒中复发的绝对风险仍然很低,设备闭塞也存在风险和副作用。最近的指南强调了知情共享决策的重要性,即评估个人受益概率和终身置入设备的风险。
然而,随机临床试验的研究水平分析通常只提供符合试验条件患者的参考级别的结果。然而,个别患者在许多方面存在差异,可能会影响受益的可能性。常规来讲,单次单因子(one-variable-at-a-time)亚组分析只能以有限的方式探讨治疗效果的异质性(HTE,heterogeneity of treatment effec),但由于患者同时在许多不同重要方面的差异,因此在多因素可信度和个体的适用性方面存在众所周知的问题。
2021年12月来自美国的David M. Kent等在 JAMA 上公布了他们对六项 RCT 试验个体参与者数据的汇总分析结果,以先前开发的评分系统为基础,评估PFO闭塞对卒中复发疗效的异质性。
SCOPE(Systematic, Collaborative, PFO Closure Evaluation)联合会的研究人员汇集了所有6项随机临床试验的个体患者数据,这些试验比较了PFO闭塞联合药物治疗与单独药物治疗对PFO相关卒中患者的作用,共纳入了3740名参与者。这些试验于2000年至2017年在全球范围内进行。
纳入的患者进行了PFO闭塞联合药物治疗或单纯药物治疗。亚组分析采用了RoPE(Risk of Paradoxical Embolism)评分(10分评分系统,得分较高反映了患者年龄较轻且无血管病危险因素)和PASCAL(PFO-Associated Stroke Causal Likelihood)分类系统,将RoPE评分与PFO高危特征(房间隔动脉瘤或较大分流)相结合,将患者分为3类因果关系:不可能(unlikely)、可能(possible)和很可能(probable)的PFO 相关卒中。

主要结局为缺血性卒中。
在57个月(IQR,24-64)的中位随访中,3740名患者出现121个结局事件。药物治疗的卒中年化发病率为1.09%(95%CI,0.88%-1.36%),器械闭塞的卒中年化发病率为0.47%(95%CI,0.35%-0.65%)(HR,0.41[95%CI,0.28-0.60])。
亚组分析显示统计上显着的交互作用。低RoPE评分低与高RoPE评分患者主要结局(缺血性卒中)的HRs分别为0.61(95%CI,0.37-1.00)和0.21(95%CI,0.11-0.42)(交互作用P=0.02)。PASCAL分类系统分类为不可能、可能和很可能的患者主要结局(缺血性卒中)的HRs分别为1.14(95%CI,0.53-2.46)、0.38(95%CI,0.22-0.65)和0.10(95%CI,0.03-0.35)(交互作用P=0.003)。2年时,PASCAL分类不可能、可能和很可能患者的主要结局(缺血性卒中)绝对风险降低率分别为?0.7%(95% CI,-4.0%至2.6%、2.1%(95%CI,0.6%-3.6%)和2.1%(95%CI,0.9%-3.4%)。
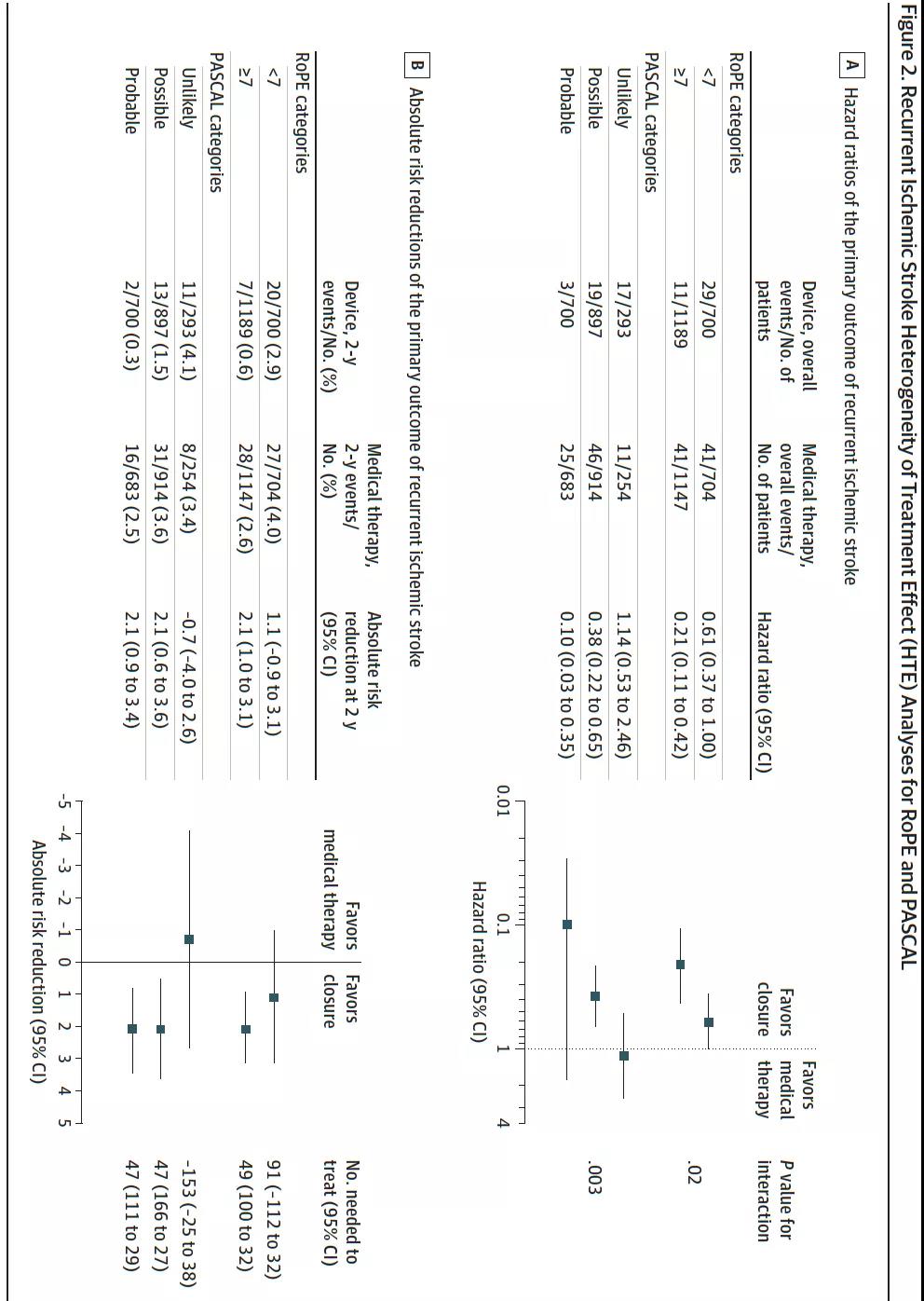
PASCAL分类不可能患者的器械相关不良事件率较高;随机45天后,PASCAL分类不可能、可能和很可能患者的器械增加房颤的绝对风险分别为4.41%(95%CI,1.02%至7.80%),1.53%(95%CI,0.33%至2.72%)和0.65%(95%CI,?0.41%至1.71%)。
最终作者认为,对于18至60岁的PFO相关卒中患者,根据卒中与PFO因果关系的概率分类,不同组别的患者采用闭塞器械降低卒中复发的风险是不同的。该分类系统具有指导个体化决策的能力。
原始出处:
David M. Kent, et al. Heterogeneity of Treatment Effects in an Analysis of Pooled Individual Patient Data From Randomized Trials of Device Closure of Patent Foramen Ovale After Stroke. JAMA. 2021 Dec 14;326(22):2277-2286. doi: 10.1001/jama.2021.20956.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











精彩评论,需要您登录查看
0
#PFO#
37
#决策#
0
好研究!
59