JAMA:偏头痛发作期静脉注射Eptinezumab的疗效评估
2021-06-22 MedSci原创 MedSci原创
对于中重度偏头痛发作期患者,静脉注射Eptinezumab可缩短头痛时间,加速令人烦躁症状消退

偏头痛的临床表现为反复发作地中重度头痛,若不进行治疗干预,症状通常可持续数小时至数天,并伴有恶心和感觉障碍。最近的研究显示,34.3%的急性偏头痛患者对治疗无应答。Eptinezumab是一种降钙素基因相关肽抗体,2020年2月FDA批准了Eptinezumab用于预防成人偏头痛,是第一个用于预防偏头痛的静脉(IV)治疗方法,在输注后第1天即可发挥预防作用。近日研究人员评估了在偏头痛发作期使用Eptinezumab的疗效和安全性。

本次研究为III期,多中心,平行组,双盲,随机安慰剂对照试验,在美国47个中心开展,招募有1年以上偏头痛病史的参与者,患者年龄在18-75岁,在筛查前的3个月里,每月偏头痛发作4至15天。患者随机接受100mg Eptinezumab治疗(n=238)或安慰剂(n=242),在偏头痛发作后1至6小时内完成治疗。研究的主要终点为头痛缓解时间,以及恶心、畏光或声音恐惧症等令人烦躁症状缓解时间,次要终点是开始输液后2小时无头痛疼痛和无烦躁症状。
患者平均年龄44岁,84%为女性,476人完成了研究。与安慰剂相比,Eptinezumab 治疗显著加快了头痛缓解(平均缓解时间:4小时vs 9小时),缩短了令人烦躁症状持续时间(2小时vs3小时)。在输注后2小时,Eptinezumab 组和安慰剂组的头痛缓解率分别为23.5% 和12.0%(组间差异11.6%;优势比=2.27) ,烦躁症状缓解率分别为55.5%和35.8%(组间差异19.6%;优势比=2.25)。在输注后4小时,结果仍具有统计学意义。Eptinezumab组治疗后24小时内使用其他止痛药物的患者比例明显少于安慰剂组(31.5% vs 59.9% ; 组间差异-28.4%;风险比0.31)。因治疗引起的不良反应发生率Eptinezumab组为10.9%,安慰剂组为10.3%,最常见的是过敏(Eptinezumab组为2.1%;安慰剂组为0%)。未发生因治疗引起的严重不良事件。
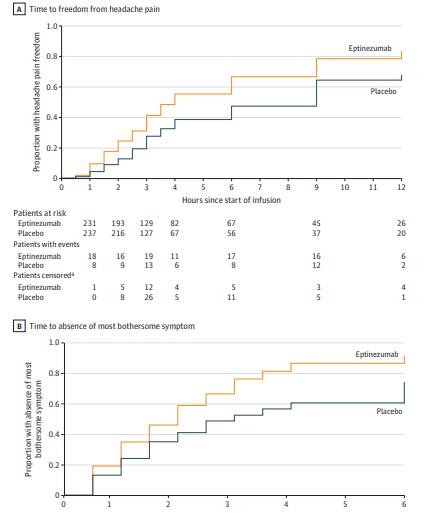
组间无头痛及烦躁症状差异
研究认为,对于中重度偏头痛发作期患者,静脉注射Eptinezumab可缩短头痛时间,加速令人烦躁症状消退。
原始出处:
Paul K. Winner et al. Effects of Intravenous Eptinezumab vs Placebo on Headache Pain and Most Bothersome Symptom When Initiated During a Migraine Attack A Randomized Clinical Trial. JAMA. June 15,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#静脉#
21
#mAb#
27
#疗效评估#
31
#Eptinezumab#
37
里总体土工
54
#静脉注射#
27
谢谢梅斯提供这么好的信息,学到很多
50
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
39
不错
56
不错
56