Front Oncol:PD-L1高表达是肝细胞癌患者手术切除后索拉非尼辅助治疗后复发的独立预测因素
2022-01-19 yd2015 MedSci原创
研究表明,PD-L1过表达可作为高复发风险肝细胞癌患者术后接受索拉非尼辅助治疗复发的独立预测因素。
近期,Frontiers in Oncology杂志上发表了一项来自四川大学华西医院团队的研究成果,主要是研究PD-1和PD-L1在肝细胞癌(HCC)患者肝切除术后接受索拉非尼治疗的预测价值。
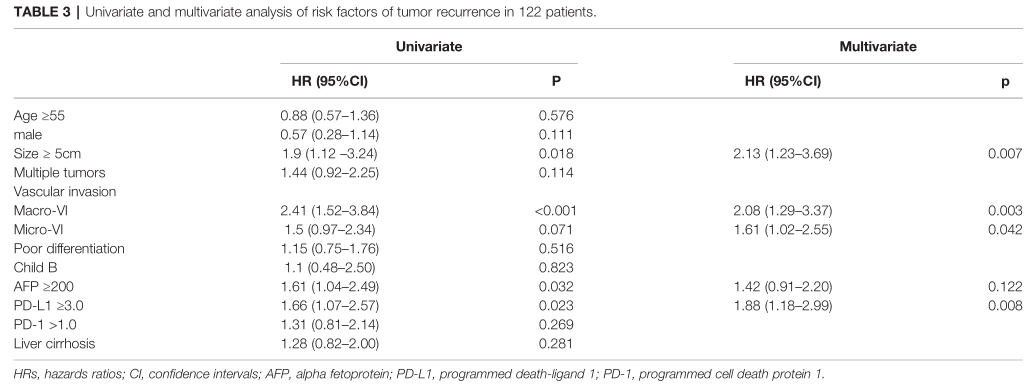
我们回顾性地纳入了在根治性切除后接受索拉非尼辅助治疗的HCC患者(N = 154),以及单独切除的患者(N = 312)。采用免疫组化方法检测PD-1在肿瘤浸润免疫细胞和PD-L1在HCC细胞上的表达。Cox比例风险模型用于探讨临床病理因素与肿瘤复发风险之间的关系。
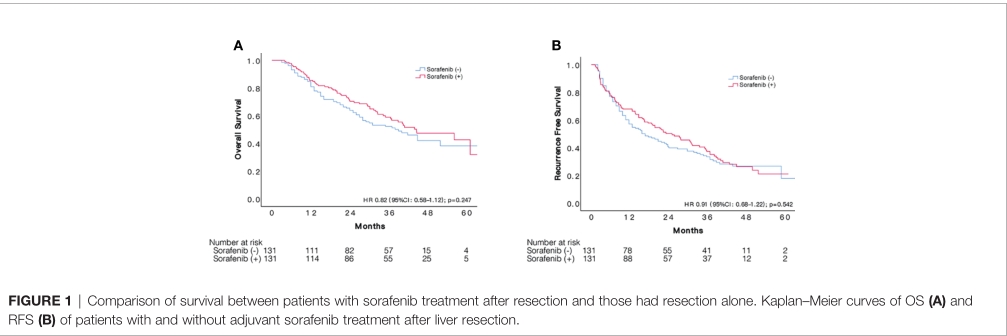
初始纳入手术+索拉非尼治疗组154例,单独手术治疗组312例,经过倾向评分匹配(PSM)后,各有131例患者。131对患者中位随访时间为35.9(+16.2)个月。索拉非尼组总体中位RFS为25.3个月(95%CI: 16.8-33.9),单独手术组为17.0个月(95%CI: 10.8-23.2),两组复发风险没有统计学差异(HR:0.92, 95%CI 0.68-1.22, p = 0.542);两组的1,3,5年RFS率分别为67.9, 38.4, 21.1% 和60.2, 34.2, 17.8%。同样,索拉非尼的加入与并不能改善患者OS (HR:0.82, 95%CI 0.58 -1.15, p = 0.542),索拉非尼组的1、3、5年OS率分别为85.5、58.9和42.6%,而单独手术组分别为84.7、52.2和38.2%。
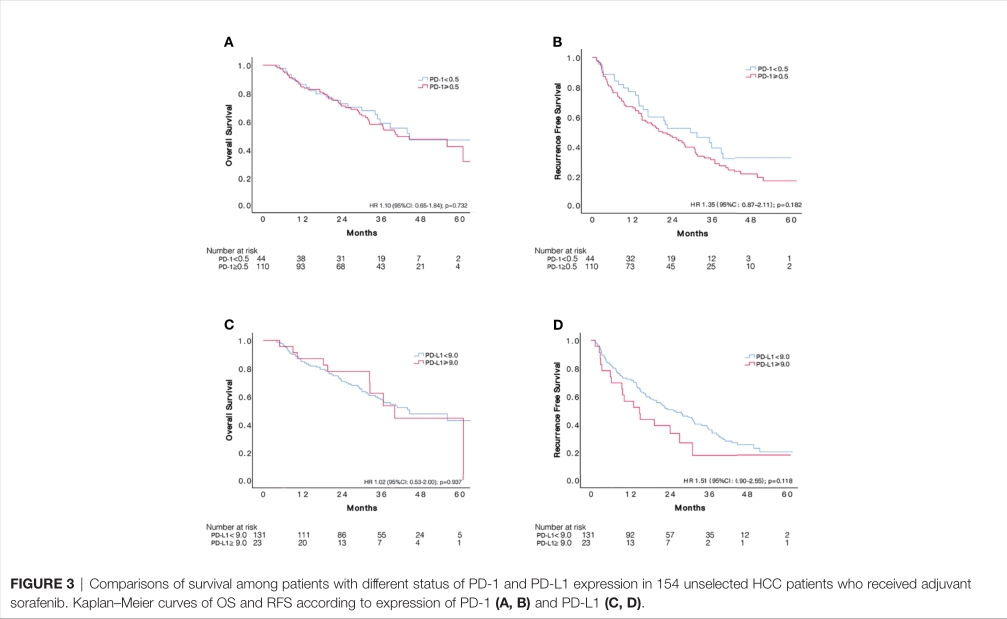
154例接受索拉非尼治疗患者中,PD-1的临界值为0.5时,110例患者定义为PD-1高表达。PD-1低表达患者的中位RFS为29.6个月 (95%CI:15.1–44.1),高表达患者的为21.2个月(95CI: 14.3–28.1),没有统计学差异 (HR 1.35, 95%CI: 0.87-2.11, p = 0.182); 同样,两组的OS类似 (HR 1.10, 95%CI: 0.65-1.84, p = 0.729)。PD-L1临界值为9时,PD-L1高表达和低表达患者的中位RFS分别为14.8个月(95%CI:7.1-22.4) 和25.3个月(95%CI: 17.1-33.5),但无统计学差异 (HR 1.51, 95%CI: 0.90-2.55, p = 0.118);同样, 两组的OS也没有统计学差异(HR 1.02, 95%CI: 0.53-2.00, p = 0.937)。
122例患者符合我们对肝癌复发高风险的定义,其中86例(70.5%)在随访期间复发。PD-1的临界值为1时,86例患者定义为PD-1高表达。PD-1低表达患者的中位RFS为 29.6 个月(95%CI: 14.9–44.3),高表达患者的为20个月 (95%CI: 11.4–28.6),没有统计学差异 (HR 1.31, 95%CI: 0.81-2.14, p = 0.267); 同样,两组的OS类似 (HR 0.94,95%CI: 0.54-1.64, p = 0.819)。
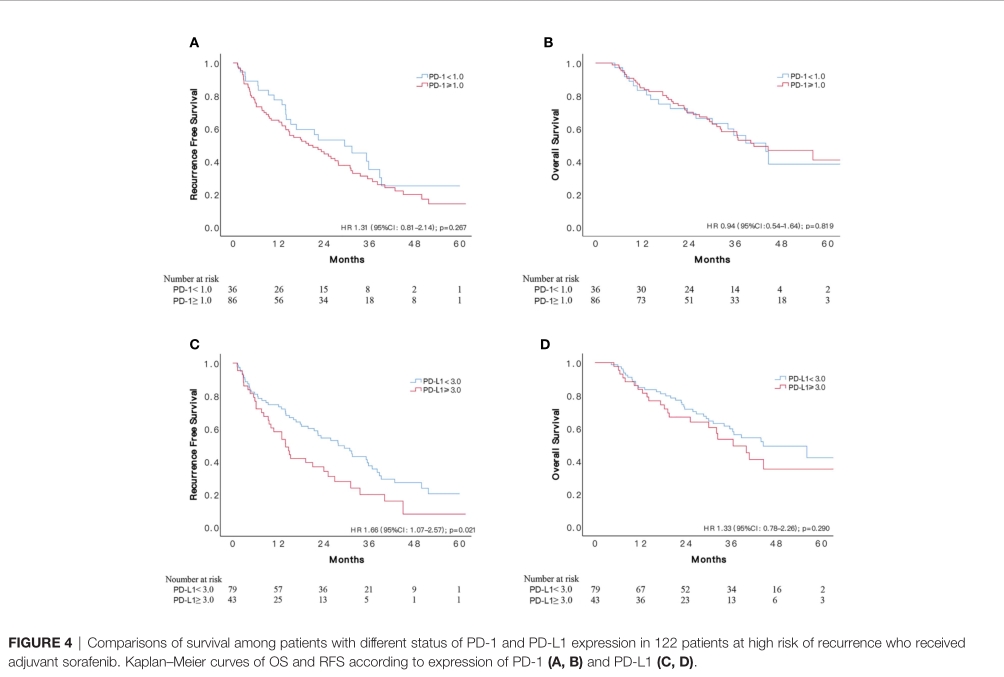
PD-L1临界值为3时,PD-L1高表达患者的中位RFS较低表达患者明显缩短,分别为14.0个月 (95%CI: 9.6-18.4)和 28.0个月(95%CI: 18.8-37.2) (HR 1.66, 95%CI: 1.07-2.57, p = 0.021);同样, 两组的OS也没有统计学差异( HR 1.33 95%CI: 0.78-2.26, p = 0.290)。但是对于未选择的154例患者中,就算PD-L1临界值为3时,两组的RFS也没有统计学差异 (p = 0.254)。
122例高复发风险患多因素分析,PD-L1高表达(HR=1.88, 95%CI 1.18-2.999,p=0.008)是RFS不良独立预后因素。
综上,研究表明,PD-L1过表达可作为高复发风险肝细胞癌患者术后接受索拉非尼辅助治疗复发的独立预测因素。
原始出处:
Tan Y, Xu Q, Wu Z, Zhang W, Li B, Zhang B, Xu X, Zhang B, Yan K, Song J, Lv T, Yang J, Jiang L, Shi Y, Yang J and Yan L (2022) Overexpression of PD-L1 is an Independent Predictor for Recurrence in HCC Patients Who Receive Sorafenib Treatment After Surgical Resection. Front. Oncol. 11:783335. doi: 10.3389/fonc.2021.783335
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肝细胞#
43
#Oncol#
35
#细胞癌#
28
#PD-L1#
26
#预测因素#
22
#手术切除#
39