JAMA Intern Med:孕期生活方式干预对妊娠期间体重过度增加及围产期不良结局风险的影响
2021-12-28 MedSci原创 MedSci原创
荟萃分析显示,产前结构化饮食和基于体力活动的生活方式干预可减少孕期体重过度增加,降低孕产妇和新生儿不良结局风险。

肥胖是世界上最常见的疾病,预计到2025年将影响到全球21%的女性。在美国,肥胖患病率更高,25%孕妇体重超标。对全球130多万名孕妇进行的荟萃分析显示,50%的孕妇妊娠期间体重过度增加(GWG)。产前生活方式干预可限制GWG,然而不同干预类型对孕产妇和新生儿结局的益处尚不清楚。近日研究人员评估不同类型的饮食和基于体力活动的产前生活方式干预与GWG、孕产妇和新生儿结局之间的关系。

本次研究为系统综述及荟萃分析研究,收集2017年2月1日至2020年5月31日,MEDLINE、Embase、Cochran相关研究,纳入标准为报告GWG、孕产妇和新生儿结局的随机试验。研究的主要终点为平均GWG降低,次要结局包括妊娠期糖尿病、妊娠期高血压、剖宫产、早产、大或小胎龄、新生儿重症监护病房入院或胎儿死亡。
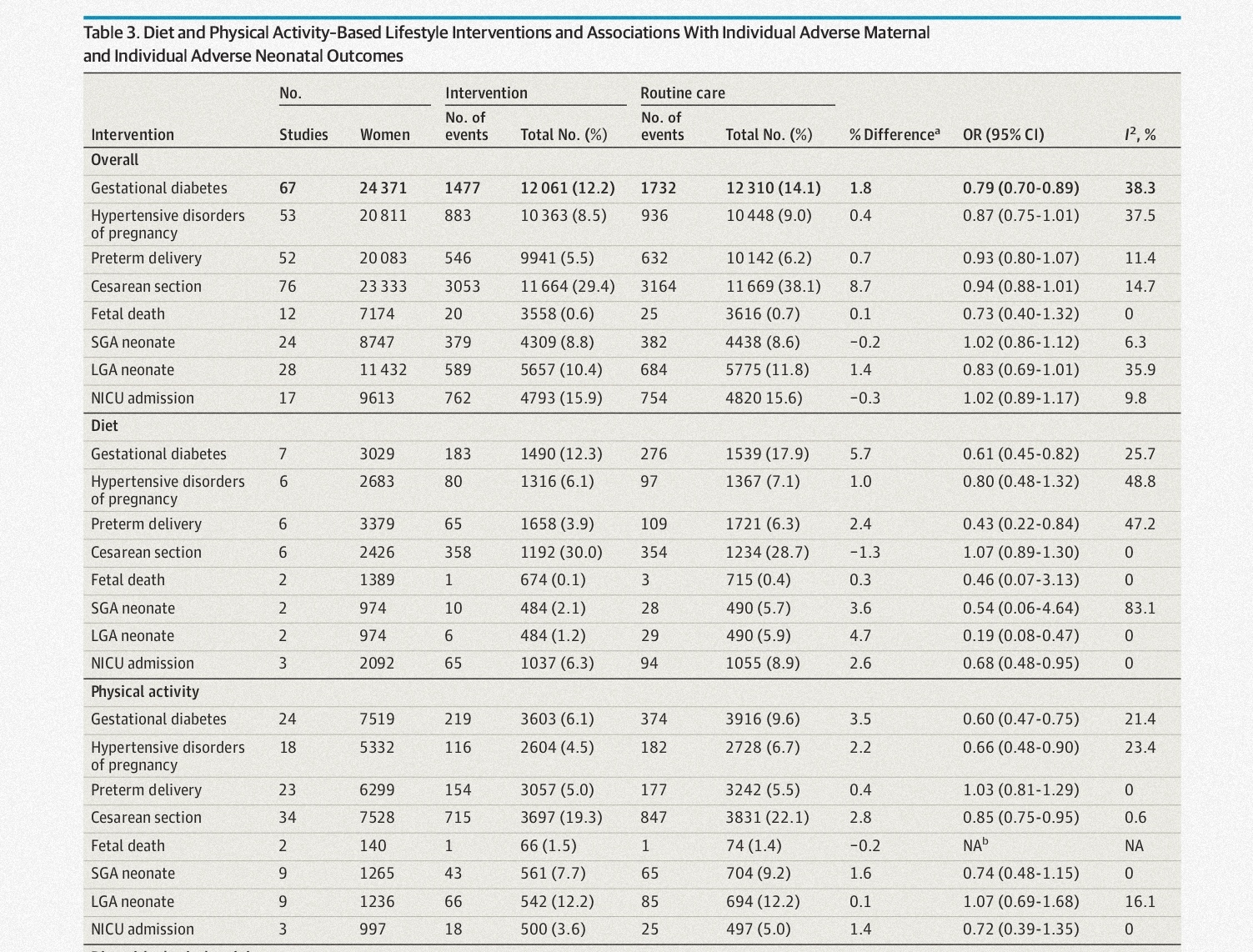
共有117项产前生活方式干预的随机临床试验(涉及34 546名妇女)。与常规护理相比,总体生活方式干预与降低GWG(−1.15kg)、妊娠糖尿病风险(优势比[OR]:0.79)和总不良孕产妇结局相关(OR:0.89)。饮食干预(−2.63 kg)对降低GWG的效果优于体力活动(−1.04 kg)或混合干预(例如,非结构化生活方式支持、带有体重监测的书面信息或单独的行为支持,−0.74kg)。饮食干预与降低妊娠糖尿病风险(OR,0.61),早产、大胎龄新生儿、新生儿重症监护入院(OR,0.68)以及总的孕产妇(OR,0.75)和新生儿不良结局(OR,0.44)相关。体力活动与降低妊娠糖尿病(OR,0.60)、高血压疾病(OR,0.66)、剖宫产(OR,0.85)和总不良孕产妇结局(OR,0.78)相关。饮食联合体力活动干预与GWG降低(−1.35 kg;)、妊娠糖尿病风险降低(OR, 0.72)和总不良孕产妇结局风险降低(OR, 0.81)相关。
体育活动及饮食干预对GWG及围产期结局的影响
荟萃分析显示,产前结构化饮食和基于体力活动的生活方式干预可减少孕期体重过度增加,降低孕产妇和新生儿不良结局风险。
原始出处:
Helena J. Teede et al. Association of Antenatal Diet and Physical Activity–Based Interventions With Gestational Weight Gain and Pregnancy OutcomesA Systematic Review and Meta-analysis. JAMA Intern Med,December 20,2021。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了
55
好
50
#妊娠期#
29
#Med#
31
认真学习了。
61