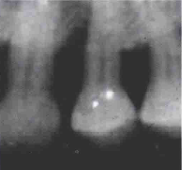
J Periodontol:引导性组织再生结合同种异体骨移植治疗骨缺损
2020-06-27 网络 网络
目前,引导组织再生(GTR)的结果的临床数据很少。这项回顾性队列研究的目的是评估GTR后的预后,稳定性以及治疗后牙齿的存活率。
目前,引导组织再生(GTR)的结果的临床数据很少。这项回顾性队列研究的目的是评估GTR后的预后,稳定性以及治疗后牙齿的存活率。
研究包括使用生物可吸收膜和骨移植替代物的GTR治疗的骨缺损以及为期1年以上的随访期。进行生存和回归分析评估预后,其稳定性和牙齿的固位。通过Cox比例风险模型和多元广义线性模型评估记录的变量对临床附着量(CAL)和牙齿存活的影响。
选择175个治疗后的骨缺损,平均随访时间为5.75±4.6年。在基线时,平均CAL为9.56±1.93 mm,平均牙周袋深度(PD)为8.41±1.42 mm。术后1年复诊时,CAL增加3.55±1.85 mm,PD减少3.87±1.87 mm(P <0.05)。经治疗的牙齿的5年和10年存活率分别为85.0%和72.7%。基线PD,吸烟和膜暴露与CAL增加显著相关,而基线CAL,年龄,维持就诊次数显著影响牙齿的存活。
在这项研究的局限性内,GTR可以提高牙齿存活率和整体临床效果,是治疗骨缺损的不错的选择。
原文出处:
Jad Majzoub,Guided tissue regeneration combined with bone allograft in infrabony defects: Clinical outcomes and assessment of prognostic factors. Journal of periodontology, 2020 June. Doi: 10.1002/JPER.19-0336
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#同种异体#
37
#骨移植#
45
#PE#
37
#骨缺损#
0
#组织再生#
28